In a recent study published in the journal Nature Communications, researchers determined the relationship between mental disorders and the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination uptake. They also explored differences in the relationship by mental disorder type, severity, and medication status.
The coronavirus disease 2019 (COVID-19) led to unprecedented morbidity and mortality globally. Despite the widespread distribution of effective COVID-19 vaccines internationally, vaccine hesitancy and rejection remain considerable. Achieving high vaccination coverage is critical for combating the pandemic. High-risk individuals, such as those suffering from mental illnesses, are more likely to get severe COVID-19 and die. However, research on COVID-19 vaccination uptake has had mixed outcomes. For example, individuals with substance use disorders and schizophrenia are known to have lower uptake, but depression and anxiety have higher rates. Furthermore, the use of anxiolytics, hypnotics, or antipsychotics is associated with decreased vaccination uptake.
About the study
In the present observational and registry-based study, researchers evaluated the impact of mental disorders on the uptake of COVID-19 vaccines.
The researchers analyzed data from the international COVIDMENT consortium (n=325,298) and Swedish registers (n=8,080,234). The COVIDMENT cohorts included the Icelandic COVID-19 National Resilience Cohort (C-19 Resilience), the Estonian Biobank (EstBB) with COVID-19 (EstBB-C19) and linked electronic health records (EstBB-EHR), the Norwegian COVID-19 Mental Health and Adherence (MAP-19) study, the Scottish CovidLife study, the Swedish Omtanke2020 study, and the Norwegian Mother, Father, and Child Cohort (MoBa) study.
The team analyzed data for the first SARS-CoV-2 vaccine uptake by September 30, 2021, and February 18, 2022. The analysis also examined the second dose uptake between November 30, 2021, and February 18, 2022. The second dose analysis included only individuals who received vaccines other than JCOVDEN.
The primary study exposure was mental illness, and the outcome was COVID-19 vaccine uptake. Secondary exposure variables included depression and anxiety. Mental disorders were ascertained using self-reports, clinical diagnosis via ICD-10 codes, and prescriptions based on ATC codes. The National Vaccination Register (NVR) provided vaccine uptake data.
The sensitivity analyses excluded electronic medical records for exposure and outcome definitions and individuals with chronic diseases. The studies explored differences related to nationwide COVID-19 vaccination policies and mitigation strategies. Poisson regressions indicated the prevalence ratios (PR), adjusted for age, gender, comorbidities, smoking habits, and prior COVID-19 history. Random effects meta-analyses aggregated the results from the COVIDMENT cohorts.
Results
Overall vaccination rates were high, with only minimal disparities in uptake due to mental illness. COVIDMENT participants demonstrated no significant differences in vaccine uptake or the occurrence of identified mental illnesses. However, Swedish register data revealed that vaccination rates were marginally lower among participants with specialist-diagnosed mental conditions, with a 9% lower uptake among those with mental illness who were not on psychiatric medications. Individuals with drug use problems had a 16% lower vaccination uptake. The findings were similar for both sexes.
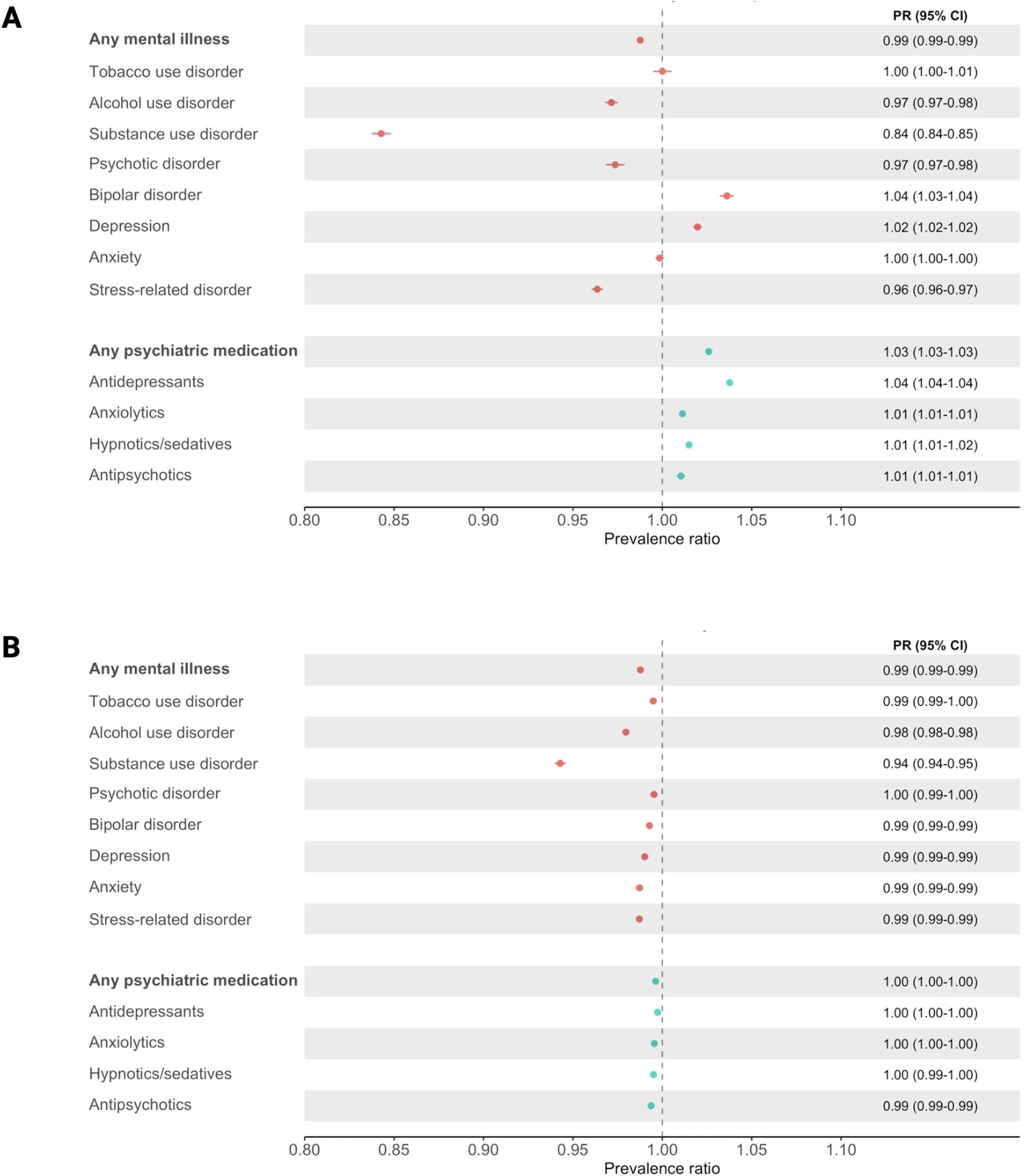 A first dose of a COVID-19 vaccine by 30th September 2021 and (B) second dose of a COVID-19 vaccine by 30th November 2021. Data are presented as PR with 95% CIs (horizontal lines), rounded to 2 decimal places. All estimates are adjusted for age, sex, region of residence, highest educational attainment, cohabitation status, income, severe COVID-19 infection and the Charlson Comorbidity Index (CCI). Substance use disorder excludes alcohol and tobacco use disorders. N = (A) 7,883,298; (B) 6,728,266.
A first dose of a COVID-19 vaccine by 30th September 2021 and (B) second dose of a COVID-19 vaccine by 30th November 2021. Data are presented as PR with 95% CIs (horizontal lines), rounded to 2 decimal places. All estimates are adjusted for age, sex, region of residence, highest educational attainment, cohabitation status, income, severe COVID-19 infection and the Charlson Comorbidity Index (CCI). Substance use disorder excludes alcohol and tobacco use disorders. N = (A) 7,883,298; (B) 6,728,266.
The COVIDMENT results showed no link between depression or anxiety and vaccination uptake. However, the Swedish register data showed a nuanced picture, revealing that individuals with specialist-diagnosed depression had higher uptake of the first dose of the vaccine, but those with depression who were not taking medication had reduced uptake for the initial COVID-19 vaccination. The findings suggest that the relationship between depression or anxiety and vaccination uptake might vary depending on disease severity and drug use. Sensitivity analysis revealed comparable findings for Nordic and non-Nordic populations.
Among COVIDMENT participants, the team noted an overall uptake of 85% for the first sars-cOv-2 vaccine, 82% among individuals with a mental disorder, and 87% among those without such disorders. Likewise, the second dose uptake rates were lower among those with a mental disorder (95%) versus those without (96%). Among Swedish registered participants, the overall prevalence of severe COVID-19 was low (0.4%); however, the prevalence was higher among individuals with mental disorders (0.8%) than those without (0.3%). The uptake of the first dose was 79% among those with mental disorders and 85% among those without such diagnosis. Second-dose uptake rates were 96% and 98%, respectively. Substance use disorders (PR, 0.84) were the most strongly associated with lower vaccine uptake. In contrast, depression (PR, 1.02) and bipolar disorder (PR, 1.04) were linked to higher vaccine uptake.
The study found that COVID-19 vaccine uptake is high across those with and without mental illnesses, demonstrating the SARS-CoV-2 vaccination campaign's comprehensiveness and success in reaching most of the population. However, the researchers discovered a significantly lower vaccination rate among unmedicated adults with diagnosed mental illness in the Swedish registry. These findings could inform the planning of current and future vaccination efforts for infectious diseases and pandemics.
Journal reference:
- Barker, M.M., Kõiv, K., Magnúsdóttir, I. et al. Mental illness and COVID-19 vaccination: a multinational investigation of observational and register-based data. Nat Commun 15, 8124 (2024), DOI: 10.1038/s41467-024-52342-1, https://www.nature.com/articles/s41467-024-52342-1