Genomics’ latest groundbreaking research, showcased at the Bupa Health Symposium, shows that a person’s genetic background is a key driver for their BMI and therefore is crucial to understanding their risk of obesity.
This new research shows that from a young age, a person’s BMI is strongly correlated with their genetics, as measured using polygenic risk scores (PRS). (See Figures A and B below.) The influence of genetics on BMI becomes more pronounced into young adulthood and middle age.
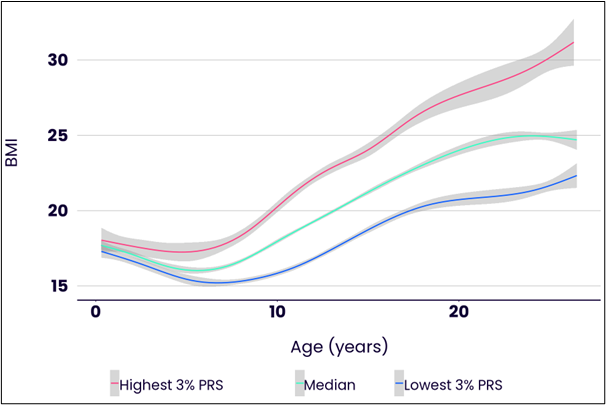
Figure A. Average BMI trajectories from birth into their twenties for individuals in different groups depending on their genetics. Those with the highest genetic scores (top 3 % of PRS) are shown in red, those with median scores in green, and those with the lowest genetic scores (lowest 3 % of PRS) in blue. The Figure is based on analysis of the ALSPAC longitudinal study which followed over 10,000 children from their birth in 1990. Image Credit: Genomics
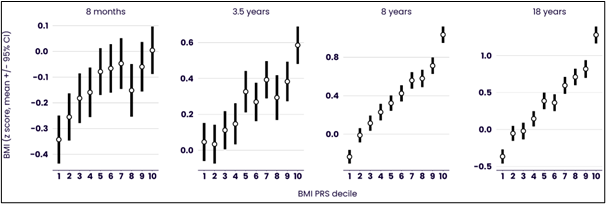 Figure B. Average BMI for ten groups of children in the ALSPAC study at different ages. The groups are the ten deciles of PRS. The leftmost point in each figure relates to the children with the lowest 10 % of PRS scores, second to left to those with the next-lowest 10 % of PRS scores, …. and the rightmost point in each figure relates to those with the highest 10 % of PRS scores. Image Credit: Genomics
Figure B. Average BMI for ten groups of children in the ALSPAC study at different ages. The groups are the ten deciles of PRS. The leftmost point in each figure relates to the children with the lowest 10 % of PRS scores, second to left to those with the next-lowest 10 % of PRS scores, …. and the rightmost point in each figure relates to those with the highest 10 % of PRS scores. Image Credit: Genomics
New research showing BMI strongly driven by genetics
By the time a child reaches their 4th birthday, their BMI is already associated with their genetics. Adults in their 20’s with relatively high PRS scores for BMI will typically experience, over the next twenty years of their lives, an increase in BMI which is three times that experienced by those with relatively low PRS scores.
Genetics impacts everyone’s BMI, from an early age and throughout their lives. But it turns out that the impact of genetics is significantly greater for people with unhealthy lifestyles, so the best way to mitigate genetics is to tackle lifestyle.
The amount of exercise a person needs to undertake to keep their BMI stable also varies a lot depending on their genetics. For example, people with relatively high genetic risk scores have to walk an average of 10,000 steps a day more to maintain a stable BMI, than do people with relatively more helpful genetics.
Amongst people who are already suffering from obesity, genetics is a powerful tool for identifying those most at risk of the serious complications associated with the condition, such as heart disease and diabetes: another set of polygenic risk scores can be used to predict the likelihood of each of these complications.
A tailored prevention and treatment solution
Understanding the genetic component of obesity risk is crucially important to supporting prevention and treatment. Research shows that a healthy lifestyle can prevent obesity and comorbidities even in individuals with high genetic risk. Much of the opportunity lies in being able to identify those for whom interventions will provide most benefit, and through tailoring advice to the needs of the individual, providing each individual with the level of support they need.
A single genetics test provides an opportunity for risk prediction for obesity, for obesity-related complications, and for many other preventable diseases. Genomics has successfully completed a trial in the NHS, incorporating the genetic element of risk for cardiovascular disease into the NHS Health Checks. Genomics’ PRS for multiple diseases will also be fed back to the millions of participants of the flagship Our Future Health programme in the coming years. Genomics is now working with Bupa Health Clinics to deploy its tests for four major diseases into its health assessments for customers in their clinics across the UK.
Obesity is the most significant health challenge of the last decade. Discussion of it must take account of the critical influence of genetics on a person’s predisposition to obesity. We need to change the discourse around being overweight, from a culture of blame and guilt to how best to help people.
Our research, and others’, shows that a healthy lifestyle can prevent obesity and comorbidities even in individuals with a high genetic risk. Those at high risk will need more support to help them stay at, or return to, a healthy weight. We have a golden opportunity to develop much more sophisticated, personalized, and successful obesity prevention programmes.
This is a great example of how including genetics in a personalized assessment of risk can allow people to become co-pilots rather than passengers on their health journey. We’re delighted to be working with Bupa to incorporate this kind of information into their health assessments for the four most preventable diseases in the UK.”
Professor Sir Peter Donnelly FRS, FMedSci, Founder and Chief Executive Officer, Genomics plc