Scientists uncover how the breakdown of a critical sugar-rich layer in brain blood vessels accelerates aging and disease—offering a new therapeutic target to restore brain health.
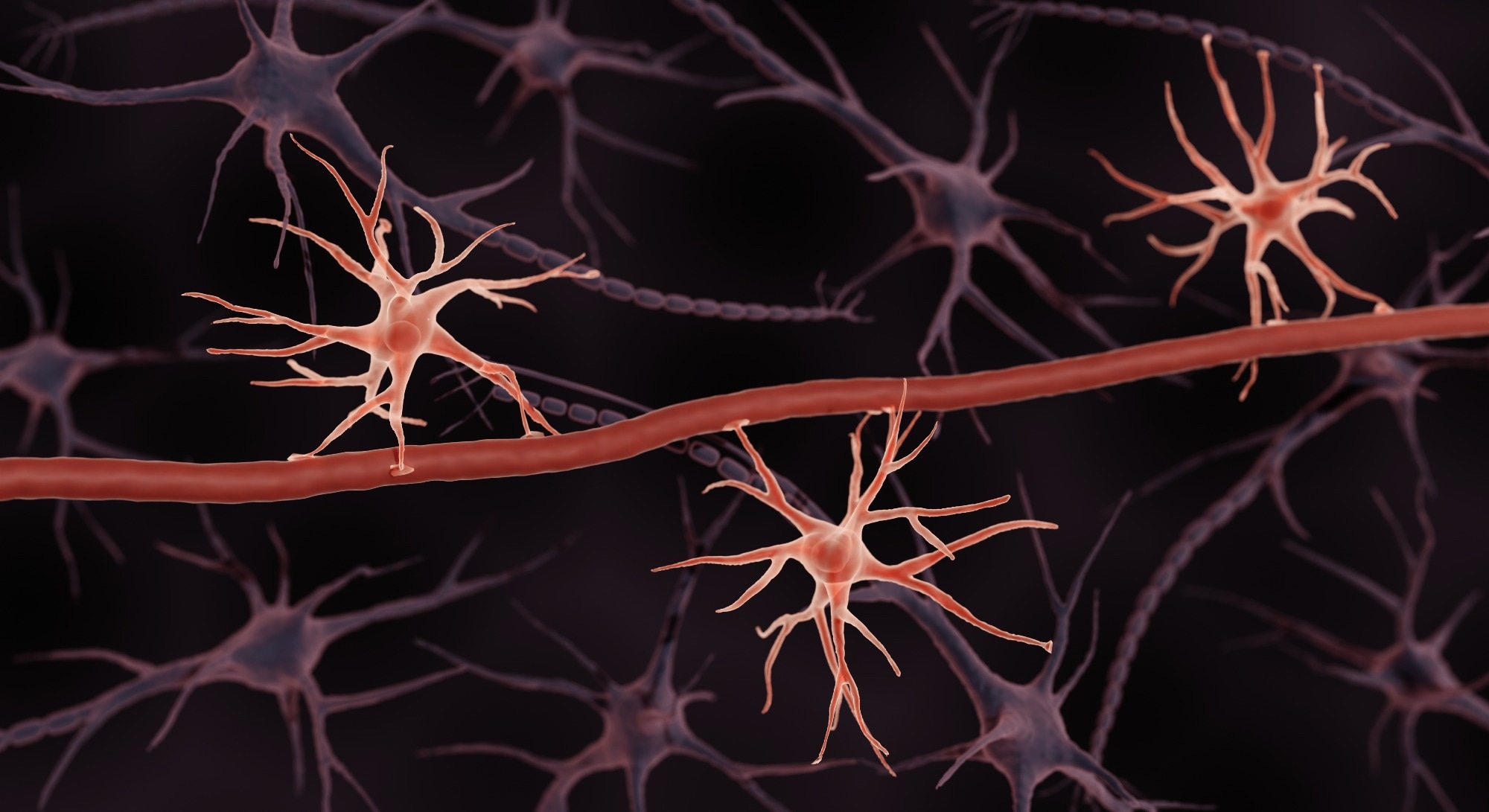 Study: Glycocalyx dysregulation impairs blood–brain barrier in ageing and disease. Image Credit: ART-ur / Shutterstock
Study: Glycocalyx dysregulation impairs blood–brain barrier in ageing and disease. Image Credit: ART-ur / Shutterstock
A recent study published in the journal Nature showed that the dysregulation of the brain endothelial glycocalyx layer impairs the blood-brain barrier (BBB) in disease and aging.
The BBB forms a highly regulated vascular interface between the brain and blood and supports brain function. The BBB’s restrictive nature is enabled by the unique properties of brain endothelial cells. In particular, mucin-domain glycoproteins within the glycocalyx play a crucial role in maintaining BBB integrity. Besides, the role of the brain endothelial glycocalyx in BBB function has been increasingly recognized.
The glycocalyx coats BBB’s luminal surface and mediates many processes, including cell signaling, transport, morphology, and adhesion. However, little is known regarding the functional roles and composition of the glycocalyx layer. BBB dysfunction is a pathological hallmark of neurodegenerative diseases and aging; however, there are no studies assessing the role of mucin-type O-glycosylation in this process.
The Study and Findings
In the present study, researchers profiled aging- and disease-related changes in the brain endothelial glycocalyx. First, they visualized the glycocalyx layers in three-month-old (young) and 21-month-old (aged) mice using transmission electron microscopy and lanthanum nitrate staining. This revealed significantly fewer luminal glycocalyx layers in aged mice than in young mice. The glycocalyx area and thickness also decreased with aging. The reduction in mucin-domain glycoproteins was particularly pronounced in the brain, while other organs, such as the heart and liver, remained relatively unaffected.
Next, the team analyzed their previous RNA sequencing (RNA-seq) dataset of brain endothelial cells from young and aged mice and found significant dysregulation of multiple glycosylation-related genes with aging. Pathway analysis revealed the downregulation of mucin-type O-glycan biosynthesis genes (B3gnt3, Galnt10, C1galt1, and Galnt2), which are critical for mucin-domain glycoprotein production, and the upregulation of heparan sulfate metabolism genes (Hs3st1, Sdc4, Gpc5, and Extl2) in aged mice.
Further, the team profiled glycosylation of brain endothelial cells via flow cytometry and imaging. Fluorescence imaging of isolated microvessels revealed significantly higher expression of heparan sulfate, hyaluronan, and chondroitin sulfate, and reduced expression of mucin-domain glycoproteins, which are essential for the structural integrity of the BBB. Cytometry analysis yielded similar results.
Next, the team evaluated the contribution of mucin-domain glycoproteins to the glycocalyx layer. To this end, they used recombinant mucin-selective proteins derived from secreted protease of C1 esterase inhibitor (StcE), a bacterial enzyme that specifically cleaves mucin domains.
The researchers used their previously developed staining reagent, StcE(E447D)-AF647, to label mucin-domain glycoproteins. This method revealed strong luminal mucin-domain glycoprotein staining in young mice but significantly weaker and more heterogeneous staining in aged mice; this age-related reduction in mucin-type O-glycosylation was specific to the brain.
Further, intravenous administration of active StcE to young mice degraded the brain endothelial glycocalyx layer, suggesting that the dysregulation of mucin-domain glycoproteins, rather than general glycan loss, leads to structural impairment of the glycocalyx layer. Additional experiments indicated that the downregulation of mucin-type O-glycan biosynthetic enzymes, such as C1GALT1 and B3GNT3, may contribute to the loss of mucin-domain glycoproteins observed with aging.
Moreover, an analysis of published single-nucleus RNA-seq datasets of Huntington’s and Alzheimer’s disease revealed that brain endothelial mucin-type O-glycan biosynthesis was a commonly downregulated pathway in both datasets. This suggests that impaired mucin-type O-glycosylation represents a shared molecular signature of BBB dysfunction across multiple neurodegenerative conditions.
Next, the researchers investigated the effects of the loss of mucin-type O-glycan biosynthesis on BBB function. To this end, core 1 synthase, glycoprotein-N-acetyl galactosamine 3-beta-galactosyltransferase 1 (C1galt1), which catalyzes an enzymatic reaction generating the “core 1 O-glycan,” was knocked down in mouse brain endothelial cells using an adeno-associated virus (AAV) targeting approach. C1galt1 knockdown resulted in increased BBB permeability and extensive leakage of immunoglobulin G (IgG) and albumin into the brain, suggesting a fundamental role in BBB stability.
Besides, immunoglobulin G (IgG) and albumin leakages were detected in the cortices, suggesting that the downregulation of core 1 mucin-type O-glycan biosynthetic enzymes increases susceptibility to BBB dysfunction and cerebral hemorrhaging. Further, the team used StcE to cleave luminal mucin-domain glycoproteins. They observed increased BBB permeability within 24 hours of StcE treatment in young mice, with prolonged exposure leading to extensive cerebral bleeding.
Moreover, the team found that overexpressing two downregulated mucin-type O-glycan biosynthetic enzymes, beta-1,3-N-acetylglucosaminyltransferase 3 (B3GNT3) and C1GALT1, in brain endothelial cells of aged mice not only improved BBB function but also significantly reduced neuroinflammation and enhanced cognitive performance. Aged mice treated with B3GNT3 overexpression showed better performance in spatial working memory and hippocampal-dependent learning and memory tasks.
Conclusions
The findings implicate the dysregulation of the brain endothelial glycocalyx layer as a molecular mechanism contributing to BBB dysfunction in aging and neurodegenerative diseases. A conserved reduction in brain endothelial mucin-type O-glycosylation was observed across aging, Alzheimer’s, and Huntington’s disease, making it a potential biomarker for BBB decline.
A decrease in this modification increased BBB permeability and susceptibility to cerebral bleeding, and also promoted oxidative stress and neuroinflammation, exacerbating brain aging and disease pathology. Conversely, overexpression of mucin-type O-glycan biosynthetic enzymes not only restored BBB integrity but also improved cognitive function, demonstrating a potential therapeutic strategy for age-related CNS diseases.
These findings suggest that restoring the brain endothelial glycocalyx may help prevent BBB breakdown, mitigate neurodegeneration, and improve cognitive resilience in aging populations.