Using real-world data from over 300,000 cases, scientists uncovered a significant link between semaglutide and reported vision problems—raising new concerns about the safety profile of this blockbuster medication.
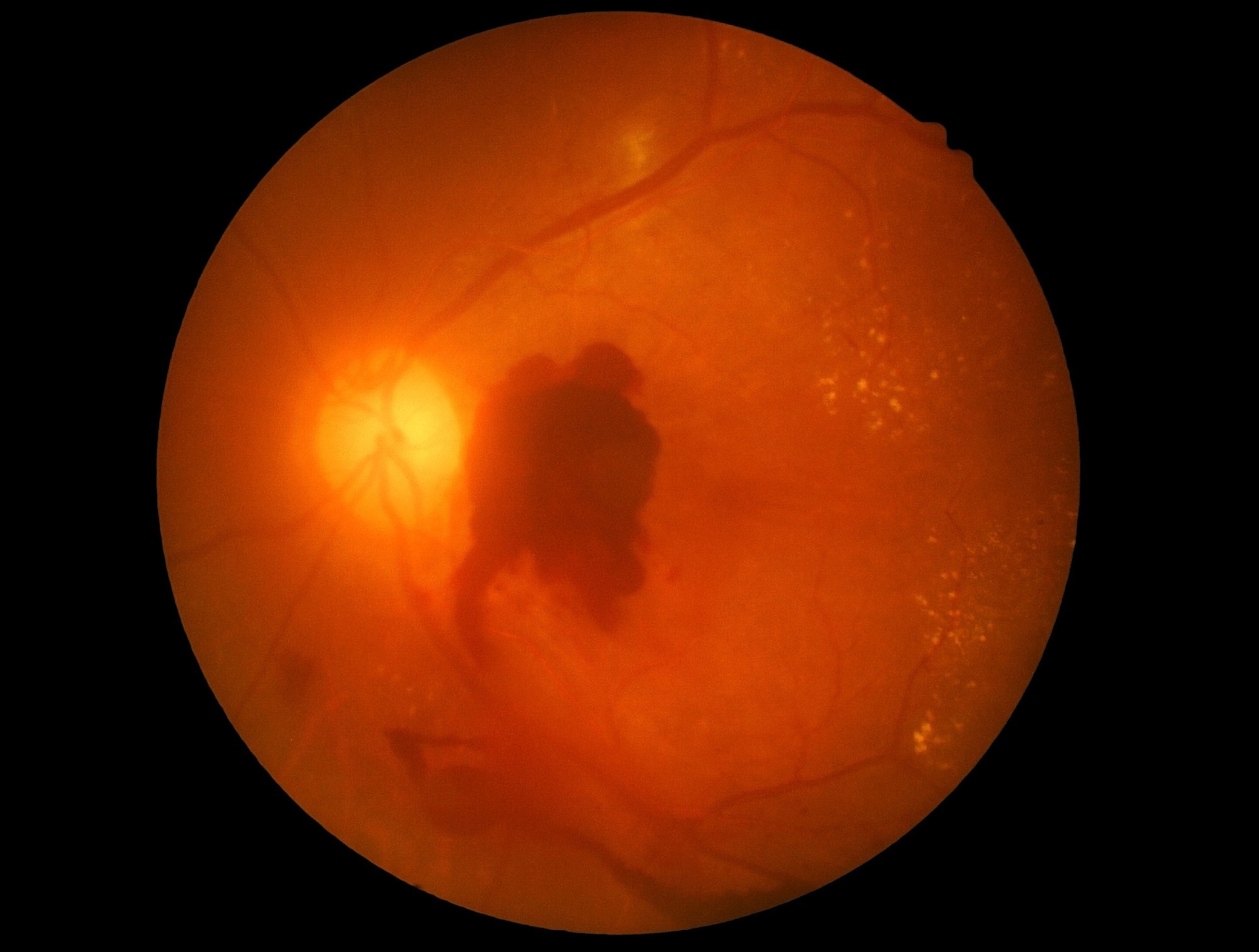 Study: Increased vision impairment reports linked to semaglutide: analysis of FDA adverse event data. Image Credit: memorisz / Shutterstock
Study: Increased vision impairment reports linked to semaglutide: analysis of FDA adverse event data. Image Credit: memorisz / Shutterstock
A team of researchers at the University of Bern, Switzerland, recently reported that the use of the antidiabetic medicine semaglutide is associated with an increased risk of vision impairment. The study findings were published in the journal BMC Medicine.
Background
Semaglutide is a widely prescribed antidiabetic medicine that acts as a glucagon-like peptide 1 receptor agonist (GLP-1 RA) for the treatment of type 2 diabetes and obesity. A 2024 study by Hathaway et al., which investigated more than 16,000 patients over a period of six years, raised ocular safety issues related to semaglutide. The study found that the medicine can potentially increase the risk of non-arteritic anterior ischemic optic neuropathy (NAION), a potentially vision-threatening condition.
The Hathaway study reported higher hazard ratios for NAION in patients with obesity (7.64) compared to those with type 2 diabetes (4.28). However, the current analysis of FDA data did not directly compare risks between these groups. Given the rapidly increasing use of semaglutide and other GLP-1 RAs worldwide, these observations warrant further investigation.
In the current study, a team of researchers at the University of Bern analyzed data from the U.S. Food and Drug Administration (FDA) Adverse Event Reporting System, a post-marketing, open-access pharmacovigilance database. The main aim was to compare the medical reports of semaglutide-related vision impairment to those associated with other antidiabetic and weight loss medicines.
Study Findings
The team analyzed 302,706 reports, including 17,853 mentioning obesity as an indication, 283,238 mentioning type 2 diabetes, and 1,615 mentioning both conditions.
The comparative analysis revealed that semaglutide use is associated with a significantly higher risk of vision impairment compared to other GLP-1 RAs. Among 11,558 semaglutide-related reports, researchers identified 417 cases specifically related to visual impairment, retinopathy, or ischemic optic neuropathy.
The researchers observed a more pronounced risk of vision impairment when comparing semaglutide with other antidiabetic medicines, including dipeptidyl peptidase-4 (DPP-4) inhibitors, sodium-glucose cotransporter-2 (SGLT2) inhibitors, and metformin.
They also noticed higher reporting of vision impairment related to semaglutide use compared to other weight loss medications, including phentermine and orlistat. The only exception was topiramate, which exhibited higher reporting of vision impairment than semaglutide (rOR 0.30, 95% CI 0.20–0.45).
Study Significance
The findings reinforce the rising concern about the risk of vision impairment associated with semaglutide use. By analyzing the FDA database, the study finds significantly elevated risks of general vision impairment, retinopathy, and ischemic optic neuropathy with semaglutide use compared to other antidiabetic and weight loss medicines.
A supplementary analysis focusing specifically on retinopathy found consistent results, with semaglutide showing higher reporting odds compared to other drugs.
Previous clinical trials that investigated the safety and efficacy of semaglutide did not report significant vision complications except for the SUSTAIN-6 trial and a subsequent meta-analysis of 23 trials, which reported a higher risk of diabetic retinopathy complications in patients receiving semaglutide. SUSTAIN-6 documented absolute rates of 3.0% for retinopathy complications with semaglutide versus 1.8% with placebo.
This discrepancy between the current post-marketing findings and prior clinical trial evidence highlights the significance of ongoing pharmacovigilance and real-world evidence studies in identifying rare but potentially serious adverse effects that may not be captured in pre-approval clinical trials.
Given the fact that diabetes is frequently associated with diabetic retinopathy and that this comorbidity can serve as a potential confounding factor, researchers separately analyzed the semaglutide-related risk of visual impairment in patients with and without type 2 diabetes.
The findings reveal that although patients with type 2 diabetes more frequently report vision impairment, the risk of impairment relative to other antidiabetic medications is more pronounced in patients receiving semaglutide.
These observations collectively highlight the need for further investigations and attentive post-marketing surveillance. Healthcare professionals should be aware of this potential side effect while prescribing semaglutide for patients with type 2 diabetes or obesity.
The study focused primarily on semaglutide formulations for diabetes (e.g., Ozempic), as data for the obesity-specific formulation Wegovy were limited.
Limitations
The FDA Adverse Event Reporting System database analyzed in this study has some limitations. The database allows voluntary data reporting from various sources, including healthcare professionals, consumers, and manufacturers, which might induce bias.
In most cases, the dataset provides incomplete health reports of patients, which might also induce bias because of prescription preferences between classes due to relevant adverse event risk factors.
The study utilized an odds ratio-based analysis approach to determine the risk of vision impairment following semaglutide use. One limitation of this approach is that medications with substantially different adverse event profiles may generate ratios that do not entirely capture their true visual impairment risk.
Moreover, the study could not provide absolute rates of vision complications with semaglutide using FAERS data, limiting clinical interpretation. However, SUSTAIN-6 trial data previously reported higher absolute rates of retinopathy (3.0% vs. 1.8%). Future studies are required to assess the absolute clinical impact of this potential side effect.
Despite these limitations, the FDA database offers real-world data on clinically relevant adverse events associated with medication use, broadening the pharmacovigilance landscape.