A pioneering clinical trial in Japan reveals that stem cell-derived dopamine neurons can survive, function, and boost movement in Parkinson’s patients, without triggering serious side effects or abnormal growth.
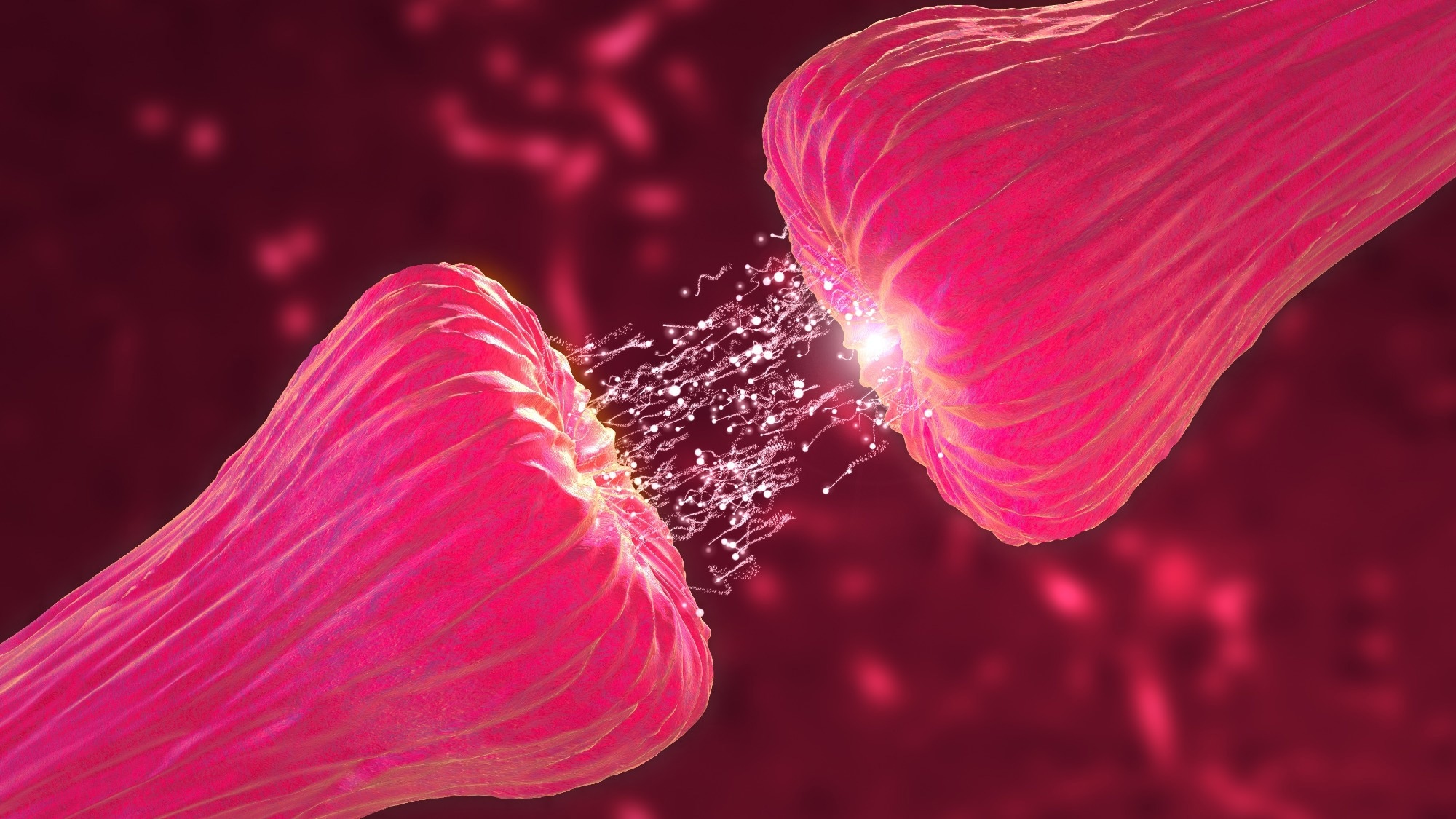 Study: Phase I/II trial of iPS-cell-derived dopaminergic cells for Parkinson’s disease. Image Credit: Cinefootage Visuals / Shutterstock
Study: Phase I/II trial of iPS-cell-derived dopaminergic cells for Parkinson’s disease. Image Credit: Cinefootage Visuals / Shutterstock
In a recent study in the journal Nature, researchers in Japan report the results of a Phase I/II clinical trial using bilateral transplantation of induced pluripotent stem (iPS)-cell-derived dopaminergic progenitors to treat Parkinson’s disease (PD). The study examined the safety and effectiveness of this cell therapy in seven patients with PD aged 50–69.
Study findings revealed the therapy’s relative safety, with no serious adverse events, including death or hospitalization, reported. While motor symptoms improved by an average of 20.4% during medication-free (OFF) periods and 35.7% during medicated (ON) periods at 24 months, these gains were not uniform: four of six patients showed OFF-period improvements, and five of six improved during ON periods.
Background
Parkinson’s disease (PD) is a chronic neurological disorder caused by the loss of dopamine-producing neurons in the substantia nigra, a brain region critical for movement control. While medications like levodopa alleviate symptoms, their long-term use often triggers complications such as drug-induced dyskinesias (involuntary movements). Early cell therapies using fetal tissue showed promise but were plagued by ethical concerns and risks of graft-induced dyskinesias (GIDs). The current study builds on preclinical work in non-human primates, where iPS cell-derived dopamine progenitors have been shown to improve motor function without inducing tumors or GIDs.
About the Study
The trial, conducted at Kyoto University Hospital, transplanted allogeneic (donor-derived) iPS-cell-derived dopamine progenitors into the putamen (a brain region affected in PD) of seven patients. Donor cells were sourced from a clinical-grade iPS cell line matched to 17% of Japan’s population via specific immune compatibility markers (HLA haplotypes). Participants were selected based on strict criteria, including age (50–69 years), disease duration (≥5 years), and responsiveness to dopamine medication. Notably, one patient (PD07) was excluded due to a COVID-19 infection and replaced with PD08.
Safety
No serious adverse events were reported. Seventy-three mild to moderate events occurred, with the most common being application site itching. One case of moderate dyskinesia was observed during medication-active (ON) periods; however, researchers attributed this to the maintained drug doses rather than the transplanted cells. Imaging confirmed the absence of tumor-like growths, and animal studies showed that the grafts contained less than 1% proliferating cells.
Efficacy
Brain scans using 18F-DOPA PET revealed a 44.7% average increase in dopamine synthesis in the putamen, with high-dose patients (5.3–5.5 million cells per hemisphere) showing a 63.5% increase compared to 7% in low-dose patients. However, improvements in motor scores did not strictly correlate with dopamine levels, suggesting factors beyond cell survival influenced outcomes.
Dyskinesia
Scores on the Unified Dyskinesia Rating Scale (UDysRS) increased by 116.4% from baseline, but these changes occurred only during ON periods and mirrored patterns of drug-induced (not graft-induced) dyskinesia. Researchers emphasized that anti-Parkinsonian medication doses were intentionally kept stable to isolate the therapy’s effects, which likely contributed to the dyskinesia increase.
Limitations and Future Directions
The study’s open-label design (no placebo group) leaves room for placebo effects, though objective dopamine synthesis measurements support biological efficacy. Long-term follow-up and autologous transplants, which utilize a patient’s own cells, could reduce immune risks and enhance outcomes. Researchers highlighted the need for larger, double-blind trials to confirm findings.
Conclusion
This trial demonstrates the short-term safety and functional promise of iPS-derived dopamine progenitors in the treatment of Parkinson's disease (PD). As lead author Jun Takahashi noted, future strategies may combine cell transplantation with gene editing or rehabilitation to optimize results.