Is post-stress sleep the key to bouncing back? Scientists reveal how the brain turns stress into restorative sleep, pointing to new strategies for mental and physical recovery.
 Perspective: Sleep and the recovery from stress. Image Credit: Hlib Shabashnyi / Shutterstock
Perspective: Sleep and the recovery from stress. Image Credit: Hlib Shabashnyi / Shutterstock
In a recent perspective piece published in the journal Neuron, researchers discussed how stress can disrupt and promote sleep and the biological mechanisms that may underlie these responses. They propose that following certain types of stress, particularly emotional or immune challenges, stress-induced sleep, especially as demonstrated in animal models, could serve as an adaptive, protective response that supports recovery by enhancing resilience, mediated by key brain circuits such as the ventral tegmental area (VTA) and lateral habenula. However, the adaptive nature of this response appears highly context-dependent and may not be universally beneficial in all scenarios.
Background
Sleep, which includes rapid eye movement (REM) and non-REM sleep, plays a critical role in human and animal health. While its exact functions remain debated, current research suggests sleep may serve multiple distinct physiological processes, not only in the brain but throughout the body. We know that sleep deprivation results in significant physiological and psychological stress.
Both humans and animals exhibit a strong drive to sleep, with prolonged wakefulness leading to severe outcomes, even death in rodents. However, stress and sleep have a complex relationship: while stress often disrupts sleep by activating arousal systems in the brain, it can also increase the body’s need for sleep.
Arousal during sleep, enabled by systems like the locus coeruleus noradrenergic pathway, is evolutionarily vital for survival. Yet, stress can over-activate these circuits, leading to fragmented sleep and reduced quality.
Most research focuses on how stress causes insomnia, but this article focuses on stress-induced sleep, a paradoxical response seen under specific conditions. Understanding this adaptive mechanism may uncover new strategies for leveraging sleep to enhance resilience and recovery from stress.
“Sickness sleep”: a stress response?
Stress is a broad biological and psychological phenomenon involving disrupted internal balance in response to perceived threats. While many stressors trigger arousal and insomnia, only certain stress types, like illness or intense emotional experiences, promote sleep.
These stress-induced sleep responses may share underlying molecular mechanisms that activate sleep-promoting brain circuits. One example is “sickness sleep,” a conserved response across species where infection or inflammation induces increased sleep.
This behavior is thought to support recovery and healing. Similarly, in rodent models, specific emotional stressors reliably trigger increased sleep.
Social defeat stress (SDS), exposure to predator scents, unpredictable chronic mild stress (UCMS), and foot shock have all been shown to increase sleep under certain conditions.
Depending on how experiments are set up, these stressors can also trigger arousal, but their ability to promote sleep is striking. The paper emphasizes that the same stressor may result in insomnia or increased sleep, depending on the experimental context, environment, and timing. This highlights the complexity of stress–sleep interactions in both animal and human research. Such findings suggest that sleep might function as a protective, adaptive response to specific forms of stress, enhancing the body’s ability to recover and cope.
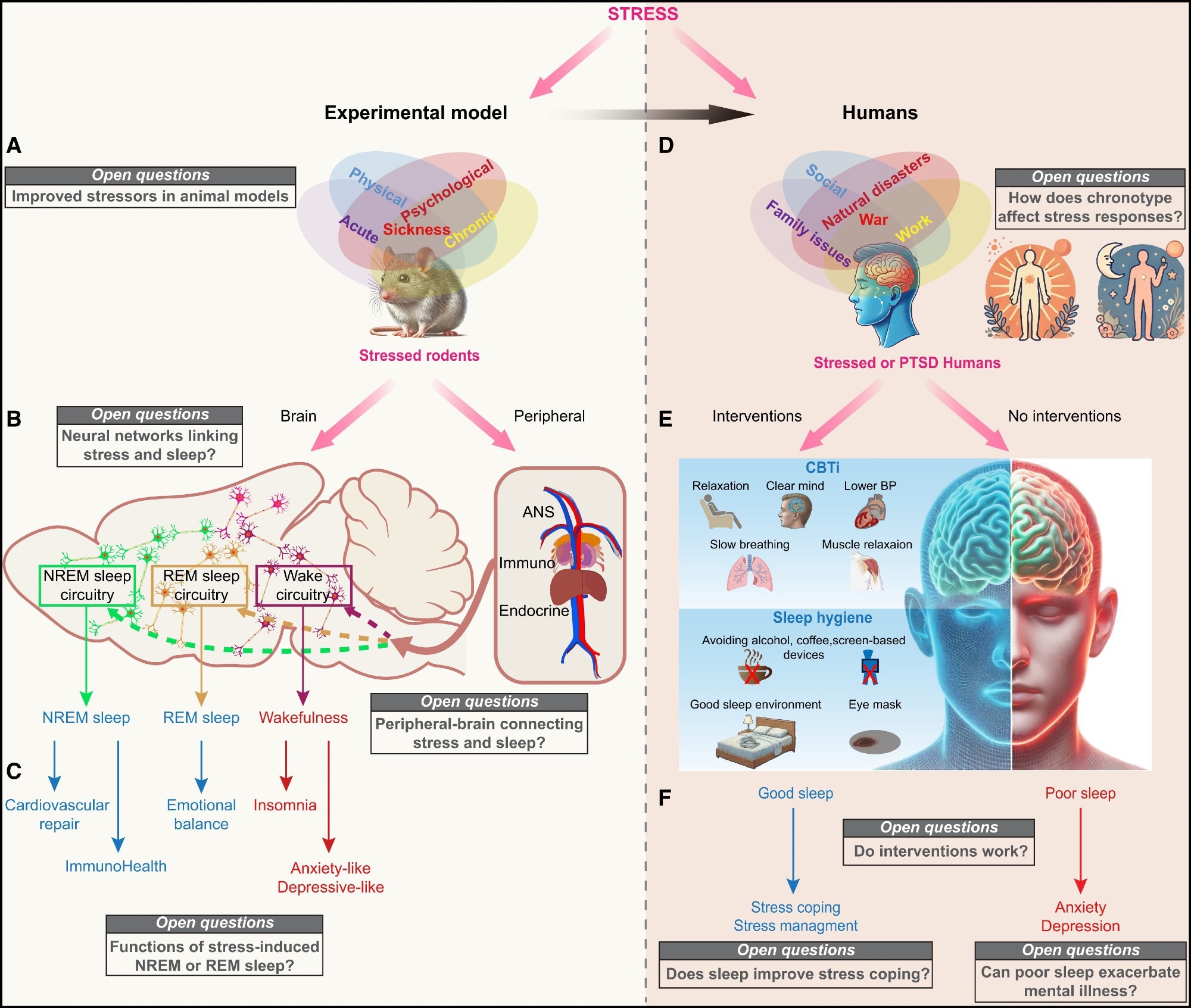 Open questions on stress-induced sleep from rodents to humans (A and B) Perspectives for rodent research. (A) Implementation of diverse stress paradigms: future research should incorporate diverse or combined stress paradigms to address both physical (e.g., injury and hyperthermia) and psychological (e.g., social defeat and unpredictability) stressors. This approach will offer a more comprehensive understanding of how various stress modalities influence sleep architecture, brain states, and behavioral outcomes. (B) Refining circuitry linking stress to brain states: the current understanding of brain-wide and peripheral-to-brain stress architecture remains incomplete. Mapping the interactions between stress-related regions and sleep-wake systems, as well as peripheral-to-brain pathways, will help identify critical hubs and circuits mediating stress responses. Advanced tools such as large-scale imaging, neural tracing, and functional manipulations are essential to elucidate these complex networks. ANS, autonomic nervous system. (C) Elucidating post-stress sleep functions: the functional significance of post-stress NREM and REM sleep remains poorly understood. NREM sleep may promote recovery by reducing autonomic activity and supporting physiological repair, while REM sleep may enhance emotional resilience through processes such as fear extinction and memory reconsolidation. Future studies should focus on delineating the distinct contributions of these sleep stages to stress recovery using integrative methods, including EEG, behavioral assessments, and targeted circuit manipulations. (D and E) Perspectives for human research. (D) The role of chronotype in stress and sleep regulation: an individual’s natural sleep-wake pattern, or chronotype, may influence their vulnerability to stress-induced sleep disturbances or sleep induction. Similarly, stress itself could alter an individual’s biological rhythm, disrupting sleep patterns. Investigating these interactions could help develop personalized interventions aligned with biological rhythms, optimizing sleep quality and stress management outcomes. (E) Targeted interventions to alleviate stress and improve sleep: can enhancing sleep quality serve as a viable intervention for stress? Approaches such as cognitive behavioral therapy for insomnia, improved sleep hygiene, or other evidence-based strategies may improve stress coping mechanisms. Understanding whether better sleep reduces vulnerability to stress-related conditions, including anxiety, depression, or post-traumatic stress disorder (PTSD), remains critical. Conversely, poor sleep following stress may exacerbate these conditions. Defining individualized treatment protocols will be essential for maximizing therapeutic benefits. (F) Sleep as a tool for enhancing stress resilience: if improving sleep quality can mitigate stress and enhance resilience, sleep interventions could become integral to managing chronic stress and preventing stress-related disorders. By prioritizing sleep health, these approaches may significantly reduce the long-term emotional and psychological burden of traumatic or chronic stress.
Open questions on stress-induced sleep from rodents to humans (A and B) Perspectives for rodent research. (A) Implementation of diverse stress paradigms: future research should incorporate diverse or combined stress paradigms to address both physical (e.g., injury and hyperthermia) and psychological (e.g., social defeat and unpredictability) stressors. This approach will offer a more comprehensive understanding of how various stress modalities influence sleep architecture, brain states, and behavioral outcomes. (B) Refining circuitry linking stress to brain states: the current understanding of brain-wide and peripheral-to-brain stress architecture remains incomplete. Mapping the interactions between stress-related regions and sleep-wake systems, as well as peripheral-to-brain pathways, will help identify critical hubs and circuits mediating stress responses. Advanced tools such as large-scale imaging, neural tracing, and functional manipulations are essential to elucidate these complex networks. ANS, autonomic nervous system. (C) Elucidating post-stress sleep functions: the functional significance of post-stress NREM and REM sleep remains poorly understood. NREM sleep may promote recovery by reducing autonomic activity and supporting physiological repair, while REM sleep may enhance emotional resilience through processes such as fear extinction and memory reconsolidation. Future studies should focus on delineating the distinct contributions of these sleep stages to stress recovery using integrative methods, including EEG, behavioral assessments, and targeted circuit manipulations. (D and E) Perspectives for human research. (D) The role of chronotype in stress and sleep regulation: an individual’s natural sleep-wake pattern, or chronotype, may influence their vulnerability to stress-induced sleep disturbances or sleep induction. Similarly, stress itself could alter an individual’s biological rhythm, disrupting sleep patterns. Investigating these interactions could help develop personalized interventions aligned with biological rhythms, optimizing sleep quality and stress management outcomes. (E) Targeted interventions to alleviate stress and improve sleep: can enhancing sleep quality serve as a viable intervention for stress? Approaches such as cognitive behavioral therapy for insomnia, improved sleep hygiene, or other evidence-based strategies may improve stress coping mechanisms. Understanding whether better sleep reduces vulnerability to stress-related conditions, including anxiety, depression, or post-traumatic stress disorder (PTSD), remains critical. Conversely, poor sleep following stress may exacerbate these conditions. Defining individualized treatment protocols will be essential for maximizing therapeutic benefits. (F) Sleep as a tool for enhancing stress resilience: if improving sleep quality can mitigate stress and enhance resilience, sleep interventions could become integral to managing chronic stress and preventing stress-related disorders. By prioritizing sleep health, these approaches may significantly reduce the long-term emotional and psychological burden of traumatic or chronic stress.
Sleep for Promoting Recovery
In animals, sleep after illness or injury (especially non-REM sleep) promotes physiological healing, such as better heart recovery. Similarly, following emotional stress, increased non-REM or REM sleep improves anxiety, social behavior, and resilience.
For example, in mice, stress-activated, sleep-promoting neurons—such as GABAergic cells in the ventral tegmental area (VTA)—reduce anxiety and promote social recovery after stress. REM sleep may help extinguish traumatic memories, with its loss increasing emotional vulnerability.
While stress is often linked to insomnia in humans, recent studies show nuanced effects. For example, social stress before sleep can increase deep sleep, and more post-trauma sleep (especially REM) may reduce intrusive memories. However, the benefits vary due to individual differences, context, and unmeasured factors like sleep architecture.
People with depression often show prolonged REM sleep. While some treatments suppress REM, animal data suggest REM may help emotional processing. This contradiction raises the possibility that REM sleep’s role depends on the context and could be both adaptive and maladaptive. The original perspective notes that while antidepressant drugs often suppress REM sleep, it is still unclear whether this suppression is beneficial, and some animal data suggest that REM sleep itself may be part of an adaptive stress recovery process.
Surprisingly, immediate sleep deprivation after trauma may reduce traumatic memory formation, as shown in both human and rodent studies. This paradoxical finding highlights that, in some contexts, delaying sleep after trauma can blunt the consolidation of aversive memories, though the mechanisms remain to be fully elucidated.
Conclusions and Unanswered Questions
Sleep following stress may aid recovery by supporting essential neurobiological processes. In animal models, resilient individuals often sleep after stress, suggesting that this response helps restore balance. However, the mechanisms linking physical tiredness, stress, and the need to sleep are still unclear, and more evidence from human studies is required.
Animal models can be improved by developing stress paradigms that better reflect human physical and psychological stress. In terms of neural mechanisms, we currently lack a comprehensive understanding of the circuits and neuromodulators that link stress and changes in sleep.
Stress likely alters hormonal and immune systems, influencing sleep in ways that are not yet well understood. Time may also be a factor, with preferences towards mornings or evenings influencing sleep recovery and responses to stress.
Overall, post-stress sleep likely aids coping and recovery, but its effects depend on stress type, timing, sleep stage, and individual factors. The article highlights several open questions, such as how chronotype affects stress-sleep interactions, how specific neural circuits mediate these effects, and whether interventions targeting sleep can reliably buffer stress-related disorders.
Improving sleep through cognitive behavioral therapy or interventions that promote sleep hygiene could buffer stress and enhance resilience. A better understanding of these interactions could shape novel treatments for stress-related disorders.