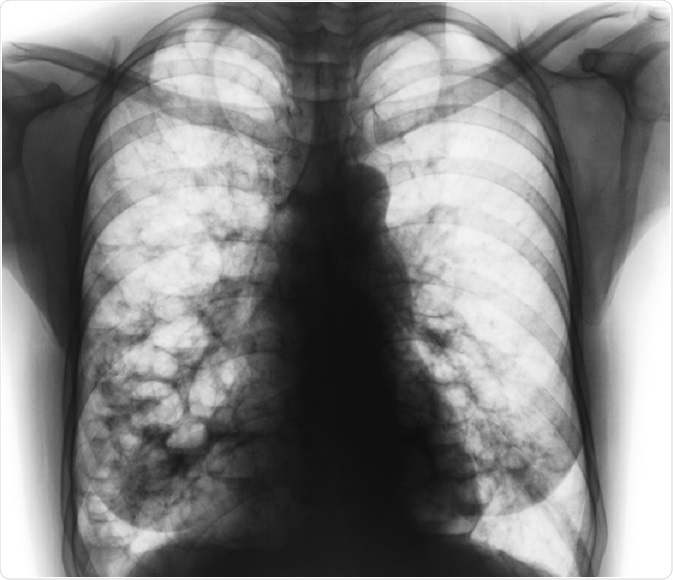
Bronchiectasis is a condition in which the airways become abnormally wide, causing mucus to build up and damage the bronchial wall. This, in turn, increases the susceptibility of the lungs to infection.
 Puwadol Jaturawutthichai | Shutterstock
Puwadol Jaturawutthichai | Shutterstock
The symptoms of bronchiectasis vary in severity from person to person, and include:
- Long-term cough that produces phlegm
- Breathlessness
Bronchiectasis may affect anyone of any age, but most commonly the middle-aged segment. Unfortunately, the damage done to the lungs by bronchiectasis is permanent.
What causes bronchiectasis?
Although in many cases a specific cause for bronchiectasis cannot be found, known risk factors include:
- A history of serious lung infections such as pneumonia or whooping cough
- A weakened immune system that leaves the bronchi susceptible to infections
- Allergic bronchopulmonary aspergillosis (ABPA) - an allergy to a specific kind of fungi that causes the bronchi to become inflamed
- Aspiration - inhaling foreign objects
- Cystic fibrosis and ciliary defects
- Connective tissue diseases
How does bronchiectasis affect the lungs?
The bronchi are small tubes in the lungs that carry air to the alveoli, from where oxygen is then absorbed into the bloodstream.
The walls of the bronchi are usually covered in mucus on the inside to protect them against damage and infection. However, inflammation can weaken the bronchi, causing airway dilatation and increased mucus accumulation. This makes the bronchi more susceptible to infections.
Infections cause more damage to the bronchi, further increasing mucus production, thereby initiating a cycle that repeatedly damages the bronchi.
Treating bronchiectasis
Although the damage to the lungs from bronchiectasis is permanent, there are a number of treatment options that aim to relieve symptoms and prevent the damage from escalating. Early diagnosis is key in limiting the amount of damage done to the lungs.
Self-care measures that patients can take to relieve their symptoms and perhaps arrest the progression of the condition include:
- Not smoking
- Having an annual flu vaccine
- Having the pneumococcal vaccine
- Taking regular exercise
- Staying hydrated
- Staying away from people with colds or the flu
- Eating a balanced diet.
Antibiotics
Antibiotics are used for lung infections. Although antibiotics for lung infections are usually taken orally, for severe infections antibiotics may be administered intravenously.
Expectorants
Expectorants are drugs that help to thin mucus. They may be taken in conjunction with decongestants to further improve results. These medications make it easier to cough up mucus. However, there is little information on their efficacy in bronchiectasis.
Chest Physical Therapy (CPT)
There are several chest exercises that patients can carry out by themselves if they are first trained in their proper performance by a physiotherapist. These exercises help alleviate coughing and breathlessness. Patients may use a downward head tilt or lie on their stomachs to improve the effects of CPT.
Active Cycle of Breathing Techniques (ACBT)
Active cycle of breathing techniques (ACBT) is a common technique. It comprises a repeating cycle of breathing exercises. The cycle starts with normal breathing, followed by deep breathing, and then coughing.
The deep breathing loosens the mucus and moves it upwards, and coughing pushes it out. The cycle is repeated for 20 minutes to half an hour. This technique is not recommended without instruction by a physiotherapist, as further lung damage may occur if the technique is carried out incorrectly.
Forced Expiration Technique (FET)
Another breathing exercise is called forced expiration technique (FET). FET involves the patient forcing out a few breaths, also known as huffing, and then taking some relaxed breaths.
A procedure called chest percussion or chest clapping can also be used to help move mucus from the airways. It involves a physiotherapist drumming the hands on the patient’s chest and back, or the same effect can be achieved with a specific device known as a mechanical percussor.
Other devices include masks that produce vibrations which help break up the mucus within the airways, inflatable vests that use airwaves to push mucus towards the upper airways, and handheld breathing devices that move mucus with vibrations. However, there is a paucity of information on the efficacy of these devices.
Bronchodilators
Bronchodilators are drugs that help relax the muscles around the airways and so make breathing easier. These medications are usually given through a nebulizer, consisting of face masks or a mouthpiece. Nebulizers pass the medicine directly to the lungs, and thus produce rapid action. Antibiotics may also be given via a nebulizer. The use of bronchodilators is sometimes recommended previous to chest physical therapy.
Oxygen therapy
Oxygen therapy increases blood oxygen levels. Oxygen is administered through the nose or via a mask. Oxygen therapy can be given at home or in hospital.
Surgery
Surgery for bronchiectasis is rare. However, in cases where surgery is necessary; for instance where there is severe bleeding in the airways, partial removal of the airway may be necessary, or a surgical procedure needed to control bleeding. In very rare cases, lung transplants may be carried out, and the unhealthy lungs are replaced with healthy lungs.
How effective are the treatments for bronchiectasis?
Some bronchiectasis treatments are adapted from cystic fibrosis (CF) and chronic obstructive pulmonary disease (COPD) therapies, as these conditions affect the same areas of the lungs and present similar symptoms. However, according to a survey carried out in the UK in 2002, 87% of physiotherapists feel the need for more disease-specific research.
Caution is necessary when using treatments prescribed for other conditions, as different conditions show varying response to the same treatment, however similar their symptoms.
Further Reading
Last Updated: Jan 10, 2019