Bronchiectasis is a chronic lung disease characterized by abnormal thickening of the airways and excessive accumulation of mucus in the respiratory tract.
What is Bronchiectasis?
Bronchiectasis is a disorder of the airways, also called bronchi, which carry air in and out of the lungs. The airways contain glands that produce mucus to prevent the airways from being dry and help trap dusts or germs that are present in the inhaled air.
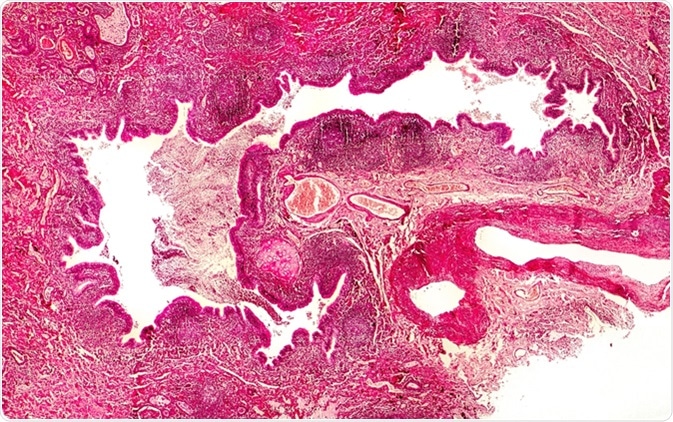
Bronchiectasis, cross-section through bronchus. Light photomicrograph showing dilatated and distorted bronchus containing pus - Image Credit: Kateryna Kon / Shutterstock
In healthy persons, mucus is removed from the airways by small hairy structures called cilia that are present in the airway linings. In bronchiectasis, thickening of the airway wall from chronic infection and inflammation causes airways to lose their ability to remove mucus. Thus, an excessive accumulation of mucus occurs and predisposes the person to infection. Bacterial infections further increase airway inflammation and further airway thickening.
What Causes Bronchiectasis?
Many factors are related to bronchiectasis.
- Genetic diseases – inherited health conditions such as cystic fibrosis (malfunctioning of glands that are responsible for secreting saliva, sweat, sebaceous, mucus, etc.) and primary ciliary dyskinesia (structural or functional abnormalities of the lungs) can lead to progressive bronchiectasis and early death.
- Immunodeficiency – humoral immunodeficiency or reduced ability of blood components (antibodies, complement proteins, etc.) to fight infections, such as those caused by bacteria.
- Lung infections – past history of severe lung infections, such as pneumonia, whooping cough, and tuberculosis.
- Inflammatory bowel disease – Crohn’s disease or ulcerative colitis.
- Rheumatic diseases – inflammatory diseases that affect the joints, ligaments, tendons, bones, and muscles, such as rheumatoid arthritis and Sjögren’s disease.
- Allergy – severe lung allergy caused by fungus, such as allergic bronchopulmonary aspergillosis.
- Airway blockage – due to aspiration of food particles into the airways.
- Other conditions – having chronic obstructive pulmonary disease (COPD) or asthma for a long time increases the risk of developing bronchiectasis.
What are the Symptoms of Bronchiectasis?
The most common symptom of bronchiectasis is coughing up sputum (thick mucus). This is often accompanied by extreme fatigue, lack of concentration, difficulty breathing, sinus problems, fevers and infections, coughing up blood-tinged mucus, chest pain, joint pain, anxiety, and depression.
How is Bronchiectasis Diagnosed?
Bronchiectasis is suspected in patients who cough up a large amount of sputum every day. Diagnostic tests that are performed to confirm bronchiectasis.
- Chest X ray – to visualize the lungs and airways
- Chest CT scan – to obtain detailed information about the location and intensity of lung damage
- Lung function tests – to check respiratory rate, amount of inhaled and exhaled air, etc.
- Blood tests – to check for diseases that may be related to bronchiectasis and measure levels of infection-fighting blood components
- Sputum culture – to check for the presence of infectious agents, such as bacteria or fungi
- Bronchoscopy – a flexible tube with a light source and a camera is inserted into the airways and images are taken to inspect the airways. This procedure is helpful in detecting blockages and sources of bleeding.
How is Bronchiectasis Treated?
The most commonly used treatments for bronchiectasis are antibiotics, hydration, and chest physiotherapy. Without proper treatment, bronchiectasis can lead to serious health complications, including respiratory failure, atelectasis, and heart failure.
- Antibiotics – oral or intravenous administration of antibiotics is the main treatment for reducing chronic and frequent lung infections. Antibiotics that reduce inflammation, such as macrolides, may be particularly helpful.
- Mucus thinning medicines – these medicines are administered through nebulizers and are used to dissolve airway mucus so that it can be coughed up easily.
- Hydration – drinking plenty of water is helpful for preventing mucus thickening.
- Chest physiotherapy – chest clapping or percussion is performed manually or using a device (such as mechanical percussor, inflatable therapy vest, or handheld vibrator) to loosen mucus so that it can be coughed up more easily. Additionally, a forced expiration technique and active cycle breathing can be used by patients to move mucus from the lower airways to the upper airways.
- Bronchodilators– used to relax airway muscles
- Oxygen therapy –to increase oxygen levels in the blood
- Surgery – This is a treatment of last resort to remove an isolated section of affected airway or to intervene when the patient has heavy bleeding related to bronchiectasis.
Further Reading
Last Updated: Dec 9, 2022