COVID-19 is a respiratory disease characterized primarily by symptoms of cough, fever, and breathing difficulties. However, there are notable symptoms that are very common in COVID-19 including the loss of the sense of taste/smell and bodily pain/aches, including headache.
Since the pandemic began in early 2020, epidemiological and case data have vastly improved our knowledge and understanding of the symptoms, disease course and treatment strategies for COVID-19.
The main symptoms of COVID-19 that distinguish it from other respiratory illnesses such as influenza (flu) and cold are the loss of the sense of taste or smell. Aside from that, there is great overlap in the symptoms of flu and COVID-19, including fever/chills, aches, fatigue, sore throat, stuffy/runny nose and headache.
 Image Credit: TANAPAT LEK.JIW / Shutterstock.com
Image Credit: TANAPAT LEK.JIW / Shutterstock.com
The prevalence of headache in COVID-19 patients varies from 10-30% in those hospitalized with COVID-19 and around 6-10% of all symptomatic patients. Whilst headache alone is not probably related to COVID-19, headache presenting alongside a fever or cough, and definitely loss of taste/smell may be a good indicator of infection.
The type of headache may also be an indicator of COVID-19. The severity of headaches in COVID-19 also varies from moderate (dull headache) to severe and could be related to the severity of infection. Those with severe headaches may present with migraine-like symptoms including throbbing or pulsing sensations and aggravation with head/neck movements.
The cause of headache in COVID-19 may be attributed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) binding to ACE2 on trigeminal nerve endings within the nasal cavity and causing trigeminovascular activation, in addition to systemic inflammation (increased cytokines). This is most likely the cause of the loss of the sense of taste and smell too. Whether these symptoms develop or not may be related to the viral load within the nasal cavity and active infection at this site close to cranial nerves, as well as the differential immune response that occurs.
Headache as a predictor of COVID-19 presentation and severity
A recent study published in The Journal of Headache and Pain, aimed to characterize the clinical presentation of headache in people with existing or new headaches and those with or without COVID-19. Patients with COVID-19 that previously suffered from headaches reported that their new headaches were different from their previous headaches (80%) with as many as 50% of those reporting completely different/novel headache presentations. This was in contrast to those with headache history without COVID-19 infection who largely reported similar headaches throughout the pandemic period to before the pandemic.
Of the COVID-19 patients who had new headaches, the most frequent severity was that of mild to moderate headaches (48%) with the most severe headaches (2%) being restricted to those in hospital. Whilst as many as half of all COVID-19 patients in this study had the typical symptoms of fever and cough, diarrhea and stomachache was present in as many as 58% and the loss of taste/smell in as many as 60%.
Interestingly, the primary trigger for headache in COVID-19 positive patients was the infection itself and drugs used to treat symptoms, whereas the primary trigger for headache in COVID-19 negative people with headache was stress and social isolation.
The higher prevalence of headache in COVID-19 patients was associated with those who had a history of bilateral headaches, those with durations over 72hrs, analgesic resistant headaches, being male (even though headaches generally were more frequent in females including a higher prevalence of migraine-like headaches compared to males), and the presence of other neurological and gastrointestinal symptoms which were all were associated with an increased risk of having a new headache with COVID-19 infection.
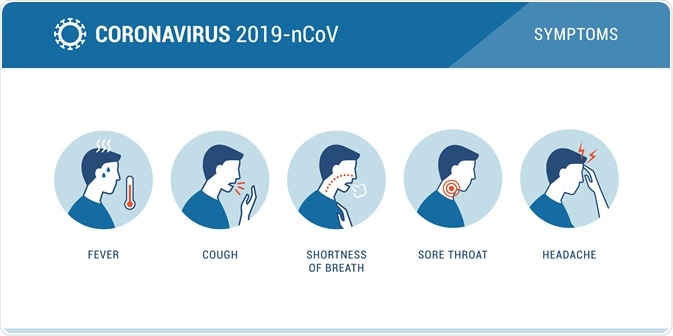 Some of the COVID-19 symptoms. Image Credit: elenabsl / Shutterstock.com
Some of the COVID-19 symptoms. Image Credit: elenabsl / Shutterstock.com
Another study published in the journal Cephalagia, mirrored many of the findings described in the previous study confirming the higher prevalence of headache in patients with the loss of taste/smell (54% vs 16%). Furthermore, headache was highly reported in younger patients compared to older (especially older male) patients. Interestingly, the presence of headache in COVID-19 was actually associated with a shorter disease duration compared to those without headache.
Furthermore, the levels of specific cytokines such as IL-6 (known to be involved in cytokine storms) were lower in those with headaches than those without and more stable if hospitalized. Finally, as many as 37% (of 130 patients) had persisting headaches 6 weeks after initial symptoms, and 21% of patients with persisting headaches reported headache as their first symptom of COVID-19. Thus, headache in this cohort subset was both the prodromal and persistent symptom relating to COVID-19.
In summary, headache is a common symptom of COVID-19 after symptoms of fever, cough and the loss of taste/smell. There is a positive correlation between having other neurological symptoms and that of headache. Some evidence has suggested that having a headache may be associated with a slightly shorter disease course and lower levels of specific cytokines. However, some patients who report headaches at the start of their infection may also suffer from persistent headaches several weeks later. More evidence is needed at this stage to definitively conclude some of these associations, as well as probing the mechanisms behind this.
References
Further Reading
Last Updated: Feb 24, 2021