Can lithium’s effect on daily activity patterns reveal who will benefit from treatment? A six-week trial finds circadian shifts emerge early, before mood improves, hinting at a biological clue to lithium response in bipolar disorder.
 Study: Effect of lithium on circadian activity level and flexibility in patients with bipolar disorder: results from the Oxford Lithium Trial. Image Credit: AtlasStudio / Shutterstock
Study: Effect of lithium on circadian activity level and flexibility in patients with bipolar disorder: results from the Oxford Lithium Trial. Image Credit: AtlasStudio / Shutterstock
In a recent study published in the journal eBioMedicine, researchers investigated the effects of lithium on circadian rest-activity in bipolar disorder (BD) patients. BD is a class of chronic mental disorders characterized by severe episodic mood changes and disturbed activity levels. Besides, disruptions in circadian rest-activity (the 24-hour cycle of motor activity dictated by the internal clock of the body) have been observed in BD. Individuals with BD often have less stable circadian rest-activity patterns, which are linked to more manic symptoms, delayed circadian phase, and higher mood variability.
Lithium remains the gold-standard BD treatment, albeit the mechanisms of action are less clear. Evidence from animals, pharmacogenomics, and cell lines suggests that lithium could influence circadian rhythms, but evidence from BD patients is still limited. Besides, lithium use has been associated with greater morningness in BD patients, although the predominance of cross-sectional studies precludes causal inferences.
About the study
In the present study, researchers examined the early effects of lithium on circadian rest-activity in BD patients. Participants aged ≥ 18 years were recruited from community mental health teams and primary care at Oxford if they were diagnosed with BD, with complaints of significant mood instability and clinical uncertainty about the benefits of lithium therapy. Individuals with contraindications to lithium, substance abuse, risk of self-harm or suicide, pregnancy, lactation, or current use of psychotropic medications were excluded. Psychiatrists assessed the intensity and frequency of participants’ mood changes before randomization. Subsequently, participants were randomized to the lithium or placebo group. The lithium group received prolonged-release tablets of lithium carbonate.
The treatment group started with 400 mg/day of lithium, with a target serum level of 0.7 mmol/L. Lithium dose was adjusted to maintain serum levels within the therapeutic range. During the six-week intervention, participants completed four assessment visits, during which serum lithium levels, treatment adherence, and adverse events were examined. Subjects completed the Positive and Negative Affect Schedule. Circadian rest-activity was measured daily using actigraphs.
Circadian rest-activity patterns were characterized using a non-parametric analysis. This analysis generated two variables, L5 and M10, corresponding to the total activity in the least active five-hour period and the most active ten-hour period, respectively. L5 and M10 onset times were also derived. A computational model (Bayesian filter) was used to differentiate between two types of variability: volatility (persistent shifts) and noise (transient fluctuations). Besides, intradaily variability (IV) and interdaily stability (IS) were calculated. Linear mixed models were used to analyze the impact of lithium on activity levels, onset times, and their variability.
Findings
Between August 2015 and January 2018, 41 individuals were screened. Of these, 35 were randomized; 19 received lithium, and 16 received a placebo. None of them experienced acute episodes warranting exclusion. L5 and M10 levels did not correlate with each other within-individual or cross-sectionally. However, the onset times of L5 and M10 were positively correlated.
M10 levels were associated with positive but not negative affect; moreover, M10 onset time was not associated with positive or negative affect. Linear mixed models showed that lithium treatment significantly reduced M10 by 18.8% in week 1, 18.1% in week 2, 27.2% in week 3, and 30.9% in week 4 compared to placebo at baseline. Notably, lithium increased the volatility (flexibility) of M10 activity levels and onset times across all weeks (Cohen’s d = 0.10–0.13, p < 0.002–0.001), suggesting a temporary adaptive destabilization that may facilitate transition to healthier patterns. The treatment also significantly increased interdaily stability (IS) by week 4 but had no effect on intradaily variability (IV) or relative amplitude.
The lithium group had a 1.5—and 1.6-hour earlier onset of M10 than the placebo group in weeks 3 and 4, respectively, but not in weeks 1 or 2; volatility in M10 onset time was also significantly higher in the treatment group at these time points. Notably, the reduction in M10 levels from baseline to week 4 did not correlate with the increase in M10 volatility. Likewise, the advancement of M10 onset time was not associated with volatility in M10 onset time.
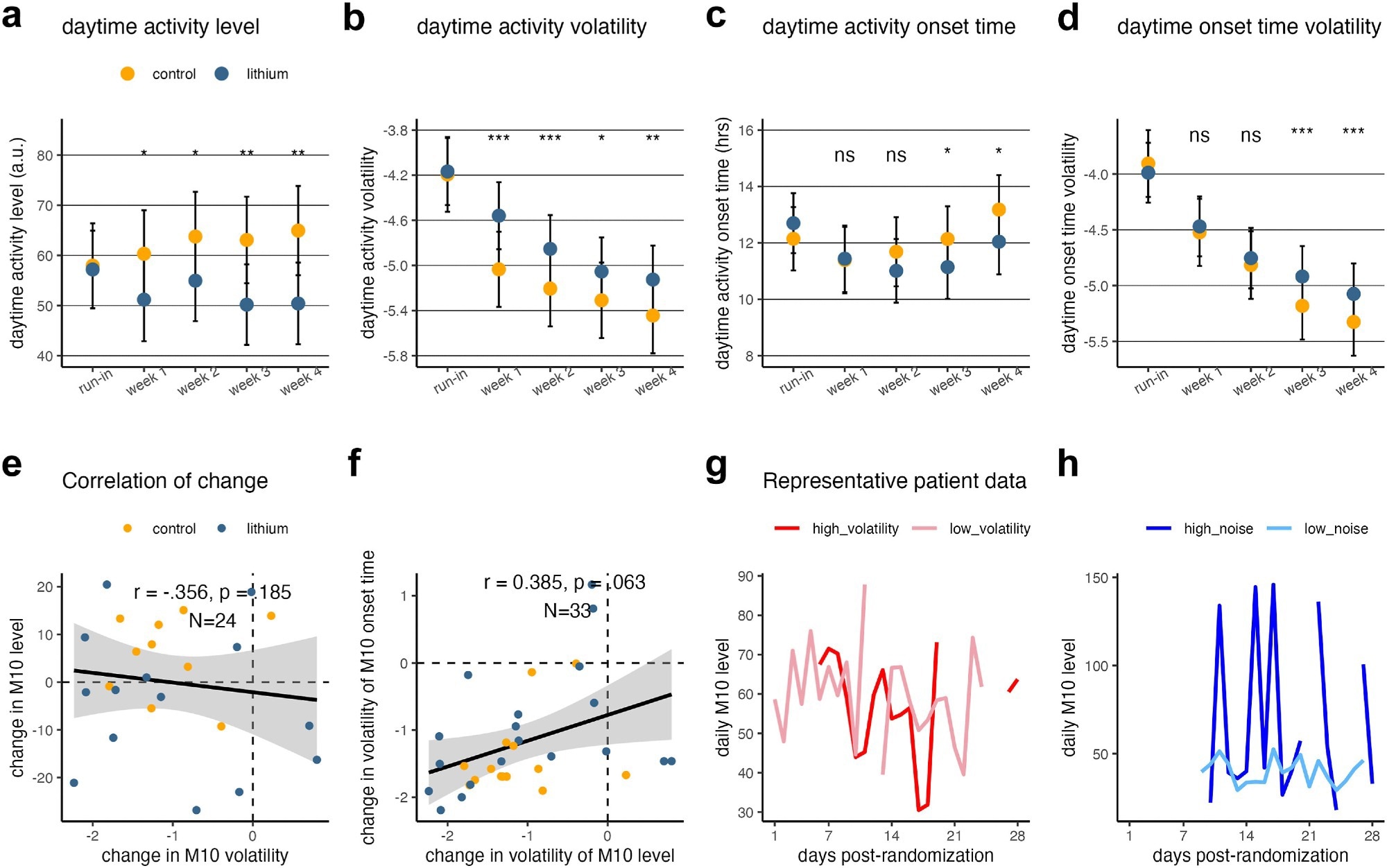 Results of the mixed linear model, for M10 level (top panel) and M10 onset time (middle panel) respectively (N = 34). (a) Daytime activity level as a function of week and group assignment. (b) Daytime activity volatility as a function of time and group assignment. (c) Daytime activity onset time as a function of week and group assignment. (d) Daytime activity onset time volatility as a function of week and group assignment. (e) The change in M10 level from pre-randomisation baseline to week 4 was not associated with the change in the change in the volatility of M10 level. (f) The change in volatility of M10 level from pre-randomisation baseline to week 4 was marginally significantly associated with the change in volatility of the M10 onset time (p = 0.06, linear mixed model). Panel F has more data points than panel E because the Bayesian filter still renders variability estimates when missing data is present. (g, h) Representative actigraphy data from a participant with higher versus low volatility (g) and high versus low noise (h). Note. The error bars in a–d indicate the 95% confidence interval; importantly, the overlap of the 95% CI of the two groups does not necessarily imply non-significance. The asterisks indicate significance level: n.s., non-significant; ∗p < 0.05, ∗∗p < 0.01; ∗∗∗p < 0.001.
Results of the mixed linear model, for M10 level (top panel) and M10 onset time (middle panel) respectively (N = 34). (a) Daytime activity level as a function of week and group assignment. (b) Daytime activity volatility as a function of time and group assignment. (c) Daytime activity onset time as a function of week and group assignment. (d) Daytime activity onset time volatility as a function of week and group assignment. (e) The change in M10 level from pre-randomisation baseline to week 4 was not associated with the change in the change in the volatility of M10 level. (f) The change in volatility of M10 level from pre-randomisation baseline to week 4 was marginally significantly associated with the change in volatility of the M10 onset time (p = 0.06, linear mixed model). Panel F has more data points than panel E because the Bayesian filter still renders variability estimates when missing data is present. (g, h) Representative actigraphy data from a participant with higher versus low volatility (g) and high versus low noise (h). Note. The error bars in a–d indicate the 95% confidence interval; importantly, the overlap of the 95% CI of the two groups does not necessarily imply non-significance. The asterisks indicate significance level: n.s., non-significant; ∗p < 0.05, ∗∗p < 0.01; ∗∗∗p < 0.001.
Conclusions
In sum, lithium treatment reduced daytime activity, advanced its onset time, and increased its volatility (interpreted as flexibility) and onset time variability. The impact of lithium remained significant until four weeks after controlling for daily affect. The authors propose that increased volatility reflects a beneficial perturbation, enabling patients to shift toward stabilized circadian rhythms.
Overall, these findings support a potential causal role between lithium and circadian rest-activity alterations in BD patients, indicating lithium’s role in enhancing circadian flexibility and advancing the daytime activity phase. The study highlights that circadian changes may precede and serve as a hypothesized mechanism mediating lithium’s mood-stabilizing effects, though larger samples and longer-term follow-up are needed to confirm this.