There are many risk factors for dementia, including Alzheimer’s disease. A majority of these are the same for cerebrovascular and cardiovascular pathologies, including obesity, hypertension (elevated blood pressure), hypercholesterolemia (elevated blood cholesterol), high sodium intake, and hyperglycemia (elevated blood sugar levels). One major risk factor, therefore, for Alzheimer’s and dementia in general is type-2 diabetes mellitus (T2DM).
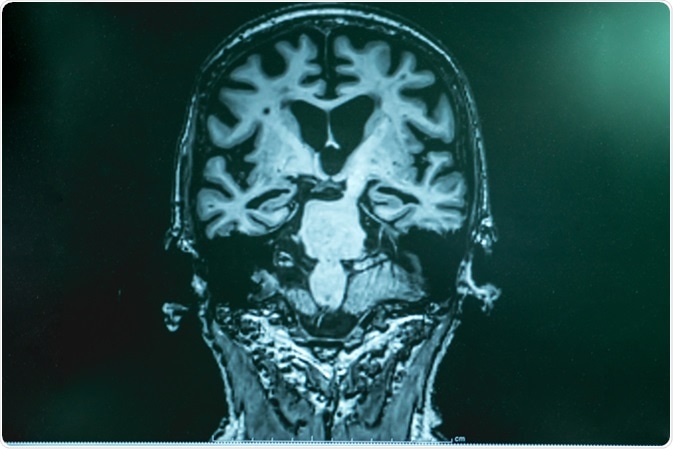
Alzheimer's disease with MRI. Image Credit: Atthapon Raksthaput / Shutterstock
What is T2DM?
T2DM is a chronic metabolic disorder characterized by hyperglycemia (high blood sugar), impaired pancreatic function (reduced insulin production), as well as insulin resistance, where the body fails to respond to insulin by other organs. T2DM is generally an age-related disorder affecting around 4 million people in the UK. The prevalence of T2DM is increasing amongst the population, as is the earlier onset of the disease due to poor lifestyle choices. Those poor lifestyle choices are also associated with increased prevalence of heart disease, stroke and dementia (including Alzheimer’s).
T2DM and Alzheimer’s – The Possible Connection
One of the main pathophysiological mechanisms that unites both diseases is that of insulin resistance. Insulin receptors have been shown to be reduced in normal aging, with even fewer receptors in Alzheimer’s patients. Insulin has many functions within the brain, such as maintaining cognition (including memory), satiety and synaptic plasticity (formation of new neural connections in memory, for example). Therefore, disruption to insulin signaling within the brain may lead to the onset of cognitive impairment seen in Alzheimer’s, in addition to potentially many other neurological conditions.
The brain is not the only organ to produce and contain beta-amyloid (one of the main Alzheimer’s proteins). The pancreas is also able to produce beta-amyloid, and is usually released alongside insulin. The toxic effects of beta-amyloid in the pancreas leads to the progressive disruption of glucose regulation in T2DM. This increase in amyloid is probably more frequent in patients with Alzheimer’s and T2DM, and not solely T2DM patients. Pancreatic amyloid does not seem to have an impact on overall cerebral amyloid levels. However, in those patients where cerebral amyloid was higher, this seems to correlate with T2DM disease onset and duration. Clearly, this relationship needs further investigation.
Finally, inflammation is often seen in obese patients, T2DM patients, as well as Alzheimer’s patients. The presence of inflammation due to T2DM and/or obesity/cardiovascular disease may in part be attributable to brain inflammation. Patients with higher inflammation tend to exhibit more cognitive deficits compared to those with lower inflammation in both the body and the brain. Animal models fed a high-fat diet tend to show marked increases in inflammation (as seen by gliosis; reactive astrocytes, and reactive microglia), within cortical and hypothalamic regions. Targeting obesity, metabolic disorders and T2DM may reduce systemic and cerebral inflammation, potentially reducing the severity of cognitive impairment in Alzheimer’s.
Treatments for Alzheimer’s Using Antidiabetic Drugs
Metformin is a commonly used drug to manage and treat T2DM. A recent clinical trial involving metformin against a placebo showed that metformin can improve cognitive deficits, such as learning and memory over a course of a couple of months. The cognitive improvements were also associated with improved brain metabolism in the frontal cortex, which is typically reduced in patients with Alzheimer’s.
Intranasal insulin is another trialed therapy in the treatment of Alzheimer’s. Compared to the placebo group, Alzheimer’s patients that were administered insulin through the nose on a daily basis showed a great improvement in memory and attention within 3 weeks. The downsides of this therapy strategy was that some patients reported headaches and nosebleeds. This therapy was particularly promising in Alzheimer’s patients with the ApoE4 allele – the most common genetic risk factors for Alzheimer’s.
In summary, whilst T2DM and Alzheimer’s disease are two distinct diseases, recent evidence has suggested common pathological mechanisms, which crossover between the two diseases, including T2DM being a risk factor for other dementias too. Furthermore, some antidiabetic drugs have shown to work to improve cognitive decline in Alzheimer’s patients. At this stage, more work needs to be done in improving our understanding of the mechanisms involved in both diseases, as well as therapies for the future.
Sources
- Akter et al, 2011. British Journal of Clinical Pharmacology 71(3): 365-76 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3045545/
- Arnold et al, 2018. Nature Reviews Neurology 14: 168-81 https://www.nature.com/articles/nrneurol.2017.185
- Jayaraman & Pike, 2014. Curr Diab Rep 14(4): 476 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3985543/
- Koening et al, 2018. Alzheimer Dis Assoc Discord 31(2): 107-113 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5476214/
Further Reading
Last Updated: Feb 26, 2019