Symptoms and clinical presentation: Fibromyalgia vs Chronic Fatigue Syndrome
Diagnosis and diagnostic criteria
Underlying causes and risk factors
Treatment and management strategies
Impact on daily life and quality of life
Conclusion
References
Further reading
Fibromyalgia (FM) consists of a chronic pain syndrome, which is characterized by pain in many parts of the body, including the skin, muscles, and joints.1

Image Credit: simona pilolla 2/Shutterstock.com
Another chronic condition called chronic fatigue syndrome (CFS), or myalgic encephalomyelitis, comprises a complex multisystem disease that is typically characterized by severe fatigue.2
Both these chronic conditions can cause difficulty in carrying out daily activities. They can be difficult to diagnose due to the lack of diagnostic tests, requiring monitoring of a patient’s symptoms for a long period before determining a diagnosis.1,2
Symptoms and clinical presentation: Fibromyalgia vs Chronic Fatigue Syndrome
Fibromyalgia symptoms predominantly include deep muscle pain in various areas of the body, similar to the feeling of a pulled muscle or bad muscle ache. Fibromyalgia pain is unpredictable and can differ from day to day, including its severity and location in the body.1
Other symptoms can include trouble sleeping resulting in restlessness, tiredness, difficulty thinking and finding words, as well as problems with concentration known as “brain fog”.1
Chronic fatigue syndrome symptoms comprise extreme fatigue, which lasts six months or longer, becomes worse with physical or mental activity, and doesn’t fully improve with rest.3
CFS symptoms can differ from case to case and from day to day, and along with extreme fatigue, may also consist of problems with thinking and memory, dizziness that worsens with transitioning from a lying down or sitting position to standing, muscle or joint pain as well as having unrefreshing sleep.3
Similar and overlapping symptoms can be found in both fibromyalgia and chronic fatigue syndrome, including tiredness, cognitive dysfunction, and muscle and joint pain.3,4
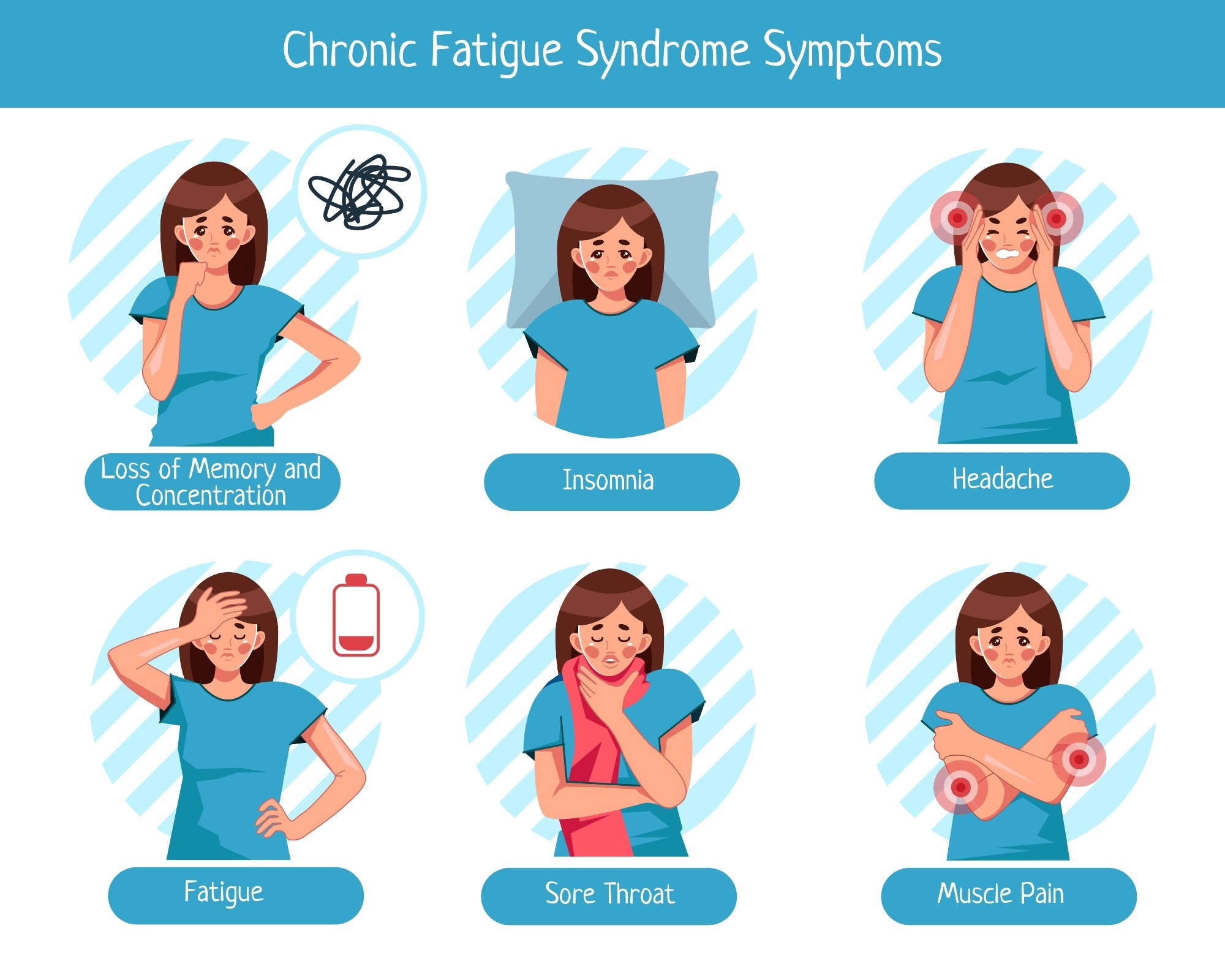
Image Credit: Lova Mikhailova/Shutterstock.com
However, differences between FM and CFS include rest having no impact on CFS and pain being experienced in many different locations at the same time for a long period in fibromyalgia patients.1,2
Diagnosis and diagnostic criteria
A fibromyalgia diagnosis consists of pain in at least 7 out of 19 specific regions of the body for the past three months, including the chest, stomach area, back, jaw, shoulders, upper arms and forearms, hips, thighs, and calves, with both sides of the body being affected.1
Additionally, other symptoms are also required to be present for three months for a fibromyalgia diagnosis, such as difficulty concentrating, exhaustion, tiredness in the morning, stomach pain, headaches, and depression.1
On the other hand, CFS is usually diagnosed after excluding other potential etiologies. The Institute of Medicine (IOM) proposed a diagnostic criterion for CFS, which includes the presence of three or more symptoms, including (i) fatigue, (ii) post-exertional malaise, and (iii) unrefreshing sleep, for more than six months.2
What is Chronic Pain?
These symptoms are required alongside an intensity characterized as either moderate or severe for a minimum of 50% of the time, as well as one other symptom, including cognitive impairment or orthostatic intolerance.2
There are some challenges with diagnosing fibromyalgia and CFS, including a lack of diagnostic tests, which can delay a diagnosis.1
Misdiagnoses may be common for both fibromyalgia and CFS due to their symptoms being associated with other conditions, such as fatigue being linked with neurological, cardiovascular, respiratory, and gastrointestinal complaints.1,2 This can lead to laboratory tests to investigate conditions such as anemia, diabetes, or an underactive thyroid.3,4
Underlying causes and risk factors
The cause of fibromyalgia, while not fully understood, has been hypothesized to be related to the way pain messages are processed in the brain, which can be triggered by a combination of factors, including genetic, physical, or psychological.1
Interestingly, fibromyalgia symptoms can begin after an event, such as experiencing physical trauma, infection, surgery, or even after significant psychological stress. However, some cases involve no single trigger, and symptoms accumulate over time.4
The etiology of CFS is also not fully understood by scientists and is controversial and complex, with theories about single versus multiple causes of the disorder, as well as the involvement of infections, the immune system, and genetic factors.2
There is increasing evidence that the pathogenesis of CFS may have a genetic component, with studies involving a family history of CFS or similar fatigue-related symptoms contributing to its development, while other theories include triggers such as the Epstein-Barr virus.2
How Fibromyalgia and Chronic Fatigue Are Related
Treatment and management strategies
Treatment for fibromyalgia includes exercise and gentle sports such as cycling, which may aid in improving wellbeing, strengthening the body, and relieving some pain.1
No one treatment can alleviate all fibromyalgia symptoms. However, a range of treatments may have an accumulative impact on the disorder.4
Pain-relieving medications, including acetaminophen, ibuprofen, and naproxen sodium, can alleviate pain and improve sleep. These medications, along with antidepressants, would be helpful for pain and depression treatment for fibromyalgia and CFS.3,4
Treatment for CFS includes medication that regulates blood pressure or heart rhythms to aid with orthostatic intolerance, which counteracts the feeling of fainting or nauseousness when standing or sitting upright.3
Other more holistic and integrative approaches for managing fibromyalgia symptoms include physical therapy, with exercises that will improve strength, flexibility as well as stamina, especially water-based exercises.4
For CFS, holistic and integrative approaches include pacing for post-exertional malaise, with the aim being to remain active without over-exertion, as patients who experience this symptom struggle to find a balance between activity and rest. Tracking your activity and symptoms can also aid in determining how much activity is too much.3
Other approaches may include avoiding caffeine or having a stable bedtime routine to aid with sleep problems, while sleep apnea machines can also be used to improve sleep.3
Impact on daily life and quality of life
With chronic fatigue being a main feature of both fibromyalgia and CFS, this can have significant implications on daily activities and the overall wellbeing of patients.5
Patients with these chronic conditions are greatly impacted by reduced social and economic interactions, as well as reduced physical function, which is more significantly reduced than expected from sedentary living.5
If patients do not utilize effective therapies for their conditions, they will continue to experience a poor quality of life and have a higher risk of health conditions associated with inactivity.5
Coping strategies often include counseling, which may help to strengthen mental resilience with approaches to managing stressful situations.4 Additionally, support from family can be helpful as depending on the severity of these disorders, it may require substantial caregiving responsibilities, as everyday tasks may not be possible for the patients.6
The ability to successfully deal with fibromyalgia and chronic fatigue syndrome may be dependent on the family’s coping skills and attitude, as a unified approach to aiding the patient with adjusting their limits and creating a stable and predictable environment with reduced stress will have a more positive effect.6
Contacting your healthcare provider to aid in dealing with FM or CFS can be helpful as well as they can provide resources that may help the patient and caregiver cope with their condition more effectively.3,4
Conclusion
Both fibromyalgia and chronic fatigue syndrome are chronic conditions that can impact the quality of life of sufferers. With no diagnostic test and no cure, they can be difficult to manage.1,2
These disorders are not fully understood; however, continued research and awareness can aid in earlier diagnoses and better treatment management, enabling patients to improve their quality of life.1,2
A 2022 study reported that the most effective way to improve cardiorespiratory fitness, as well as muscle mass and function, is by regular, intense exercise. Interestingly, future studies may investigate whether regular, intense exercise familiarizes patients with afferent signals from exercising limbs to improve exercise tolerance by reducing their increased sensitivity to effort and fatigue.5
Patients who experience relevant symptoms for more than a couple of months should seek support and professional guidance to manage their pain and fatigue more effectively.3,4
References
-
InformedHealth.org [Internet]. Overview: Fibromyalgia. Institute for Quality and Efficiency in Health Care (IQWiG). 2006. [Updated 2022 May 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK492993/
-
Sapra A, Bhandari P. Chronic Fatigue Syndrome. StatPearls [Internet]. [Updated 2023 Jun 21]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557676/
- Mayo Clinic. Chronic fatigue syndrome - Symptoms and causes. Mayo Clinic. Published 2018. https://www.mayoclinic.org/diseases-conditions/chronic-fatigue-syndrome/symptoms-causes/syc-20360490
- Mayo Clinic. Fibromyalgia. Mayo Clinic. Published October 26, 2021. https://www.mayoclinic.org/diseases-conditions/fibromyalgia/symptoms-causes/syc-20354780
- Fabio Zambolin, Duro-Ocana P, Faisal A, et al. Fibromyalgia and Chronic Fatigue Syndromes: A systematic review and meta-analysis of cardiorespiratory fitness and neuromuscular function compared with healthy individuals. PLOS ONE. 2022;17(10):e0276009-e0276009. doi:https://doi.org/10.1371/journal.pone.0276009
- Roadmap for Chronic Fatigue Syndrome & Fibromyalgia | ME/CFS & Fibromyalgia Self-Help. www.cfsselfhelp.org. Accessed June 30, 2024. https://www.cfsselfhelp.org/library/roadmap-chronic-fatigue-syndrome-fibromyalgia#:~:text=CFS%20and%20fibromyalgia%20touch%20every%20aspect%20of%20life%3A
Further Reading
Last Updated: Jul 17, 2024