Using data from the RECOVER-Adult study, a research team from the United States (U.S.) evaluated the prevalence and incidence of ME/CFS among individuals recovering from COVID-19, identified key symptoms, and compared them to uninfected individuals to better understand post-COVID health outcomes.
Background
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating condition that is often triggered by infections. Research shows that certain viruses, including Epstein-Barr and Ross River, may lead to ME/CFS, which is characterized by chronic fatigue, post-exertional malaise, cognitive impairment, and a lack of restful sleep.
The global emergence of COVID-19 has heightened concerns about its long-term health impacts, collectively termed post-acute sequelae of COVID-19 (PASC), or long COVID. Studies have revealed fatigue as a common symptom among long COVID patients, along with cognitive issues and post-exertional malaise — symptoms that also align with a diagnosis of ME/CFS.
Despite this overlap, data quantifying ME/CFS incidence after COVID-19 remains limited. This gap in knowledge hinders a comprehensive understanding and management of ME/CFS in post-COVID patients. Furthermore, the identification of PASC symptom clusters highlights a wide spectrum of symptom burden, including one particularly severe cluster associated with ME/CFS. Investigating these associations is also essential to guide healthcare strategies, improve diagnostic criteria, and develop interventions targeting this complex, multifaceted condition.
About the Study
In the present study, the team used data from the RECOVER-Adult cohort, which was part of a longitudinal, observational investigation conducted across 83 U.S. sites. It included adults diagnosed with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and uninfected individuals as controls.
The participants were classified into three groups: those who were enrolled within a month of the infection (acute infected), those enrolled after 30 days (post-acute infected), and uninfected participants with confirmed negative SARS-CoV-2 tests. The study excluded individuals with pre-existing ME/CFS.
The researchers collected data using self-reported symptoms and comorbidities recorded during study visits every three months. A diagnosis of ME/CFS was based on the Institute of Medicine (IOM) clinical criteria, with persistent fatigue, post-exertional malaise, unrefreshing sleep, and cognitive or orthostatic symptoms lasting six months or longer as requisites for a positive diagnosis. Additionally, specific questionnaires were used to assess symptom severity, including assessments of cognitive impairment.
The study also identified four distinct symptom clusters among participants with PASC, ranging from mild to severe. Cluster 4, the most symptomatic group, included severe post-exertional malaise, fatigue, cognitive impairment, and other symptoms, aligning closely with ME/CFS. Most ME/CFS cases fell within this cluster.
Furthermore, the study used statistical analyses such as propensity score matching to minimize bias between infected and uninfected cohorts. The incidence rates of ME/CFS were calculated by comparing new diagnoses in acutely infected individuals to those in matched controls.
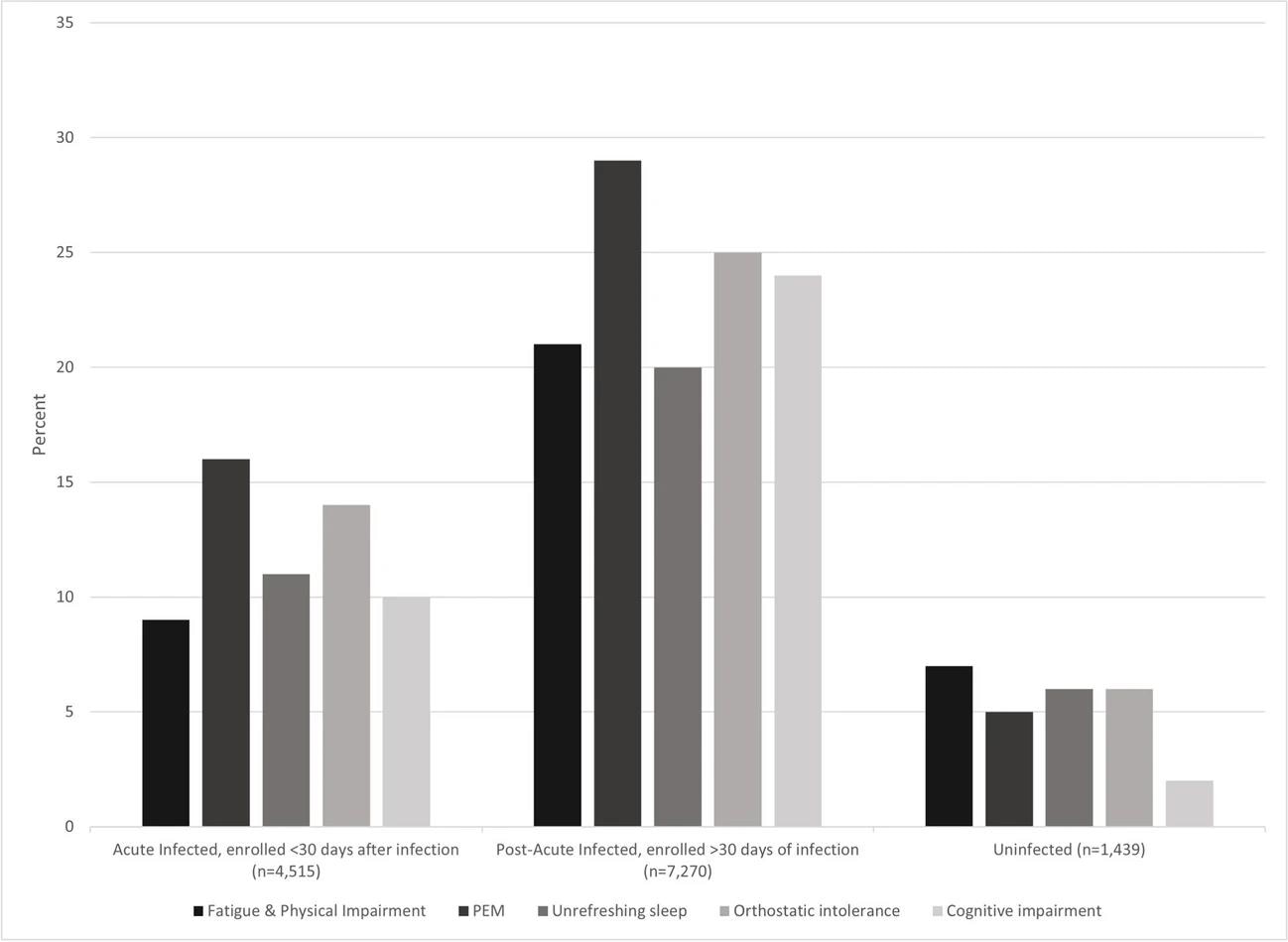
Percent of infected and uninfected participants with ME/CFS symptoms
Key Findings
The results indicated that SARS-CoV-2 infections significantly increased the risk of developing ME/CFS. Among the infected participants, 4.5% had symptoms that matched the ME/CFS diagnostic criteria six months post-infection, significantly higher than the 0.6% observed in the uninfected controls.
Additionally, the incidence rate among the acutely infected individuals per 100 person-years was 2.66, which was also significantly higher than the rate of 0.93 observed among the uninfected participants.
The most common symptom in infected individuals was post-exertional malaise, which 24% of participants reported. Other frequently reported symptoms included cognitive impairment, unrefreshing sleep, and fatigue—all aligning with the diagnostic criteria for ME/CFS. Moreover, the symptom prevalence was markedly higher in post-acute participants than in acute cases, highlighting the progressive nature of post-infectious symptoms.
Eighty-nine percent of participants diagnosed with post-COVID-19 ME/CFS were also categorized as having long COVID, with the majority assigned to PASC Cluster 4, the most symptomatic subgroup. This underscores a possible overlap between severe PASC and post-COVID ME/CFS.
The study reported a fourfold increase in the risk of developing ME/CFS in individuals who had SARS-CoV-2 infections compared to uninfected individuals. The findings also emphasized the importance of recognizing ME/CFS as a significant post-COVID sequela and implementing targeted healthcare interventions.
Conclusions
Overall, the study suggested that SARS-CoV-2 infection substantially increases the likelihood of developing ME/CFS, especially among individuals with long COVID symptoms. The results also indicated a higher risk of ME/CFS among COVID-19 patients who were older, female or had pre-existing conditions associated with pain.
The study authors noted several limitations, including reliance on self-reported symptoms, possible recall bias, and the exclusion of hospitalized COVID-19 cases. However, these limitations were balanced by the study’s rigorous methodology, including early enrollment and frequent follow-ups.
These findings emphasized the need for early recognition of ME/CFS symptoms following SARS-CoV-2 infections, improved diagnostic criteria, and comprehensive care strategies to address this debilitating condition.
Journal reference:
- Vernon, S. D., Zheng, T., Do, H., Marconi, V. C., Jason, L. A., Singer, N. G., Natelson, B. H., Sherif, Z. A., Bonilla, H. F., Taylor, E., Mullington, J. M., Ashktorab, H., Laiyemo, Adeyinka O, Brim, H., Patterson, T. F., Akintonwa, T. T., Sekar, A., Peluso, M. J., Maniar, N., & Bateman, L. (2025). Incidence and Prevalence of Post-COVID-19 Myalgic Encephalomyelitis: A Report from the Observational RECOVER-Adult Study. Journal of General Internal Medicine. DOI:10.1007/s11606024092909, https://link.springer.com/article/10.1007/s11606-024-09290-9