Fibromyalgia is a condition in which there is pain all over the body, localized to the somatic muscles. This is experienced as soreness over certain points on pressure, in the form of a dull ache which has been present for at least 3 months at the time of diagnosis. The tenderness should be elicited over different points located over all the body quadrants.
Other symptoms include insomnia, morning stiffness, tension headaches, pain and stiffness of the temporomandibular joints, depression, problems with concentration and menstrual difficulties.
In many cases there are also bowel symptoms. These may range from bloating to diarrhea and abdominal pain. In fact, about a third of patients with fibromyalgia also have irritable bowel syndrome (IBS), while bowel movements are irregular in 8 out of every 10 patients.
The symptoms often occur initially after a traumatic event, including physical or psychological disorders, but may also occur insidiously. The ratio of men to women is low.
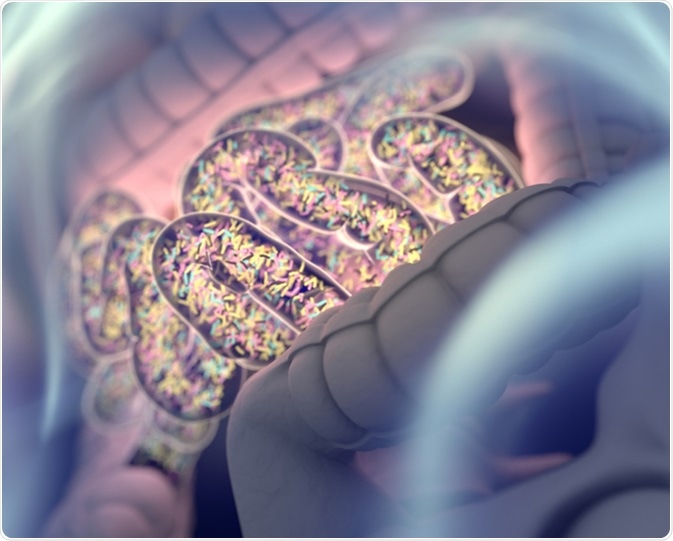
Gut bacteria , gut flora, microbiome. Bacteria inside the small intestine, concept, representation. 3D illustration. Image Credit: Anatomy Insider / Shutterstock
Fibromyalgia and the Small Intestine
IBS has been linked to the occurrence of small intestine bacterial overgrowth (SIBO), a condition in which the normal colonic flora overgrow into the small intestine to varying extents, causing disruption of normal intestinal bacterial patterns. This connection would seem to reveal that fibromyalgia is associated with SIBO as well, in light of the finding that correcting the latter by appropriate antibiotic therapy leads to clinical improvement of bowel symptoms as well in these patients.
Mechanisms of Fibromyalgia in SIBO
Several studies show that both fibromyalgia and IBS yield abnormal lactulose breath tests (LBT). The LBT is a test for bacterial overgrowth and is positive in almost all fibromyalgia patients. It is thought that endotoxins produced by overgrown bacteria are responsible for the hyperalgesia by increasing pain perception in the body.
Another mechanism of pain production is bacterial translocation, which is common in SIBO. This results in the production of endotoxins which provoke the production of the tumor necrosis factor, leading to systemic effects.
While fibromyalgia and IBS have many common features as regards the bowel disturbances, it is also true that their clinical features show significant variation.
This may be due to differences in the host, but this requires further research to be validated. It is also possible that different patterns of bacterial overgrowth may occur in different conditions, and this accounts for the variation in symptomatology.
For instance, hydrogen breath testing in individuals with fibromyalgia show a much higher level of hydrogen production compared to subjects with IBS even when both are LBT positive, and this may reflect a larger number of small intestinal bacteria.
Treatment of Gut-Related Fibromyalgia
Since modern research has shown significant correlations between the presence of fibromyalgia and increased intestinal permeability, which is related to SIBO, many healthcare providers feel that the following measures may be helpful.
Including these foods in the diet:
- Fermentable fiber such as yam and sweet potato in the diet
- Fermented foods such as sauerkraut and kimchi
- Foods rich in glycine such as tough cuts of meat
- Probiotics
Avoiding the following:
- Antibiotics and indigestible or irritating foods
- Stress
- Restricted sleep
The relationship between these disorders is still poorly understood and more work is necessary to elucidate the role of the gut in provoking this condition.
The gut flora: You and your 100 trillion friends: Jeroen Raes at TEDxBrussels
References
Further Reading
Last Updated: Jun 19, 2019