Normally childbirth involves labor pain which crescendos around the time of delivery. This significant level of pain can require much endurance from a woman, particularly if the labor takes longer than usual. This is why pain management becomes important during labor and delivery.
Knowing what options are available helps the woman and the support personnel, as well as the medical team, to decide on which should be used. This is one reason why a birth plan is useful. However, the plan should be flexible so that the means adopted can change depending on the need.
Some important ways in which a woman about to go into labor can manage her pain include:
- Being informed about the various phases of labor and what can be expected in each; this increases the feeling of control which itself reduces the level of fear and tension, and helps patients take wiser decisions under proper guidance (antenatal classes and getting information from doctors can help a lot in becoming knowledgeable about labor)
- Relaxation and breathing exercises help women to stay calm during the pain of labor
- Having the freedom to stay upright and move around, adopting different positions to ease the pain, helps birth to proceed more smoothly and allows more patient control over the process
- Having a supportive person throughout the process is a must, whether this is a midwife or a family member or friend who has been trained to support the laboring woman
- Sometimes a massage is helpful in reducing the pain
- Hot or cold packs on the abdomen or back often reduce the level of pain
- Water baths or hydrotherapy; the use of a water bath filled with water at a comfortable temperature during labor often helps lessen the pain of the contractions, but this may not be a universal experience
Entonox or nitrous oxide inhalation
A mixture of oxygen and nitrous oxide gas helps to reduce the pain of labor though it will not eliminate it. It is possible for the woman to use it herself with ease, with a mouthpiece. If this is the plan, it is wise to familiarize the patient with its use so that she can find out if she is comfortable with the feeling of the mask. It works fast in about two-thirds of women who use it, reducing the pain in about 20 seconds, provided the woman takes slow deep breaths.
Adverse effects are nil, but sometimes it may cause the patient to feel sick or drowsy. This feeling passes away as soon as its use is ceased. Some women also feel claustrophobic with the mask, which is why this technique is not suitable for them.
Pain-relieving medications: analgesics
Medications used to manage pain during birth may be classified as analgesics and anesthetics.
Analgesics do not block nerve conduction but relieve pain to a large extent. They may be systemic or local, depending on the area over which analgesia is produced.
Systemic analgesia used during labor is administered intravenously or intramuscularly. Patient-controlled analgesis is a type of intravenous analgesia in which the woman can choose the frequency and dose of medication she receives. Systemic analgesics such as diamorphine and pethidine are given intramuscularly, into the buttocks. They act within about 20 minutes and their effect lasts for 2-4 hours. They induce relaxation and relieve feelings of distress, and they usually do not inhibit labor.
Systemic analgesia may have side effects such as nausea, sedation, and disorientation. Anti-nausea drugs are, therefore, given alongside to reduce the nausea. The maternal sedation may make it difficult to push during the second stage of labor. Fetal sedation may also prevent successful early breastfeeding.
Moreover, the response to these drugs varies between women, so the initial dose may be halved to study the intensity of action before going on to the full dose. Systemic analgesics such as pethidine may cause temporary deceleration of the fetal heart and suppress neonatal respiration if given shortly before birth. However, antidotes are available to reverse this action on the fetus.
Pain-relieving medications: anesthetics
Anesthetics suppress nerve conduction and so completely prevent pain feelings in the treated area. Both local and systemic anesthesia may be used.
Local anesthesia uses injections to achieve numbness for a time over a focal area of the body. The injections paralyze the nerves nearby. Pudendal block is given just before delivery occurs. This reduces the pain as the baby moves down the vagina and stretches the perineum. Local anesthesia is also used in the perineum and vulva when an episiotomy is about to be made, or before repair of a vaginal tear.
On the other hand, regional anesthesia refers to the blocking of sensation from a region of the body. In labor, the sensations from the waist and below are blocked using various techniques such as epidural block, spinal block, as well as combined spinal-epidural anesthesia.
Epidural anesthesia
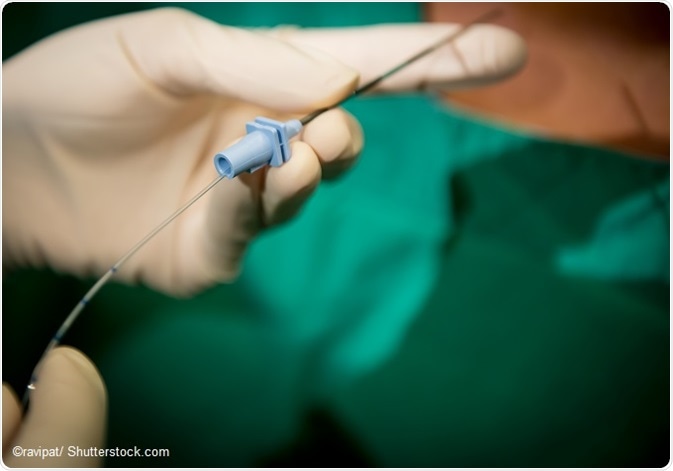
Epidural anesthesia refers to the administration of a mixture of opioid and anesthetic drugs through a slender cannula passed into the space between the spinal cord and its coverings. It paralyzes the nerve roots that make up the pelvic nerves carrying pain from the pelvic organs. It can be administered only by an anesthetist, so it will not be available during home delivery.
It is generally considered safe and very effective in pain management. It is not considered to increase the risk of Cesarean delivery, and it obviates the need for separate analgesia during episiotomy or its repair.
However, it may increase the total time of labor, may inhibit the impulse to push in the second stage and thus increase the need for assisted birth, and causes numbness and immobility of the lower limbs while its action lasts. Urinary retention may also occur till its effects wear off, so that a catheter may become necessary.
It is also associated with back pain in some women for a short while following delivery. It requires continuous monitoring of labor progress as well as of the fetal heart rate, often using fetal scalp electrodes. Rarely, maternal hypotension may occur.
TENS - transcutaneous electrical nerve stimulation
TENS refers to transcutaneous electrical nerve stimulation. In this procedure electric current is transmitted from a battery through skin electrodes. The skin stimulation blocks pain fibers from deeper in the body and also stimulates endorphin production.
It is especially useful for some women in blocking out the pain of labor contractions. However, active labor is usually difficult to filter out by such means, so its use is maximum in early labor. Its use is safe for both mother and baby.
Alternative methods
Acupuncture, acupressure, aromatherapy, hypnosis, and homeopathy are some of the alternative techniques used for pain management, but scientific research is lacking to prove or disprove their effectiveness.
Some of these should be performed only if the practitioner has a license to practice. The hospital should also be informed of the patient’s choice and trained experienced personnel should be available at the time of labor.
References
- https://www.healthdirect.gov.au/pain-relief-during-labour
- https://medlineplus.gov/ency/patientinstructions/000587.htm
- http://www.acog.org/Patients/FAQs/Medications-for-Pain-Relief-During-Labor-and-Delivery
- https://www.betterhealth.vic.gov.au/health/healthyliving/childbirth-pain-relief-options
- http://www.nhs.uk/conditions/pregnancy-and-baby/pages/pain-relief-labour.aspx
- https://www.nichd.nih.gov/health/topics/labor-delivery/topicinfo/Pages/pain-relief.aspx
Further Reading
Last Updated: Jun 14, 2019