Epileptic seizures happen when there is a burst of neural activity that leads to the physical symptoms of a seizure. The basis for seizure onset is generally an excitatory overload coupled with decreased inhibition leading to bursts of excessive neuronal discharge in the brain.
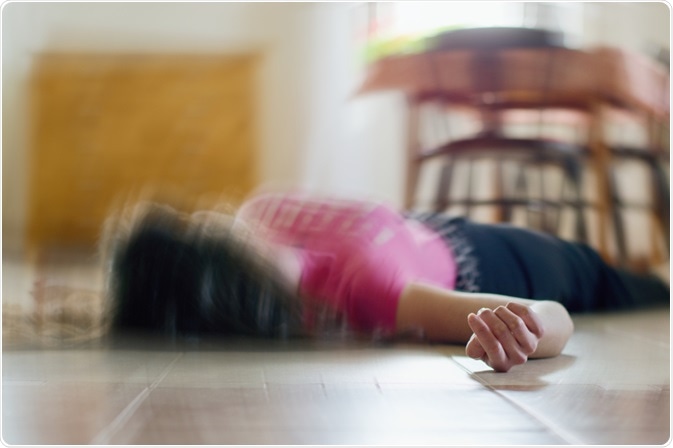
Image Credit: Tunatura/Shutterstock.com
Other forms of seizures can occur due to injury, infection, substance abuse, and hypoxia. Understanding the mechanisms behind epileptic seizures has led to many successful anti-epileptic drugs and is continuing to lead to better and improved medications for a variety of epileptic syndromes.
Epilepsy and Seizures
Epilepsy refers to a group of fairly common long-term conditions where individuals suffer from recurrent and spontaneous seizures. Seizures are characterized as spontaneous bursts of neural electrical activity within the brain that leads to temporary symptoms of a seizure.
Symptoms of an epileptic seizure can vary depending on where in the brain the seizure has occurred and how much it has spread. Thankfully, in most cases, anti-epileptic medications can successfully manage seizures, and in some cases, childhood seizures subside in adolescence.
Seizures can be characterized as simple partial (focal) with auras, complex partial (focal), and tonic-clonic seizures. Depending on the seizure type, symptoms can vary considerably.
Common symptoms of a seizure can include the uncontrollable jerking and shaking of limbs or the body (known as a fit). Some individuals may lose awareness and may stare blankly into space.
Many individuals who suffer from seizures may also experience some strange sensations such as unusual smells or tastes or a tingling feeling in the limbs.
Whilst epilepsy is usually referred to as the long-term chronic condition, seizures can also be brought on by several other factors in those that do not suffer from epilepsy. These can include stroke, brain tumors, head injuries, specific brain infections, and drug abuse (such as cocaine and MDMA).
For those that suffer from epilepsy, though the seizure can be spontaneous, there may be common triggers including lack of sleep, stress, alcohol, medications, periods, and in some rarer cases, flashing lights.
The Molecular Basis for Epileptic Seizures
The basis for any seizure is the excessive and hypersynchronous electrical discharge of neurons. This means that neurons become overly active and collectively over-fire.
Typically, this happens because there is an imbalance between neuronal excitation and inhibition in the brain (i.e. more excitation and reduced inhibition), causing excitatory overload.
This can be due to a variety of factors, especially due to genetic mutations leading to altered function and expression of excitatory and inhibitory receptors and ion channels.
The causes of such an excitatory-inhibitory imbalance in the brain can be caused due to a variety of factors including mutated genes encoding channels, receptors, or specific subunits as well as downstream signaling pathways.
These can either be at the receptor level (such as defects to GABA receptor subunits) to mutated ion channel function e.g. potassium and sodium channels.
A majority of epilepsy cases start in younger ages during childhood when the brain is still developing where the excitatory function is more prominent than an inhibitory function of synapses, hence why the young brain is more susceptible to seizures.
Some specific syndromes are caused by specific genetic changes:
- Benign Familial Neonatal Epilepsy (BFNE) is caused by mutations to a voltage-gated potassium channel encoded by KCNQ2 and KCNQ3 that are involved in the inactivation of these potassium channels, whereas dysfunction leads to increased neuronal excitability. However, these seizures do resolve with age despite the genetic mutations being present throughout life.
- Febrile Seizures Plus (FS+) also known as generalized epilepsy with febrile seizures (GEFS) is caused by defects in the α1 subunit (missense mutations) of the voltage-gated sodium channel (Nav1.1) encoded by SCN1A.
- Dravet Syndrome is similar to FS+ in the sense that it is usually caused by haploinsufficiency of SCN1A (severe mutation) leading to more severe epilepsy. Mutations to SCN1A may lead to abnormal sodium channels in cortical interneurons allowing the increased firing of excitatory pyramidal neurons that are disinhibited.
- Childhood Absence Epilepsy (CAE) is a complex polygenic disorder, but some mutations occur within CACNA1H (encoding T-type calcium channels). CAE starts within the thalamus due to increased neuronal excitability.
Other epilepsy syndromes are caused by other structural, physiological, and metabolic causes:
- Temporal Lobe Epilepsy (TLE) is caused by hippocampal scarring (direct lesions to the hippocampus) that often need surgical interventions. Seizure genesis is thought to be due to impaired GABAergic inhibition as well as enhanced synaptic excitation through novel axonal sprouting.
- West Syndrome is caused by hypoxia-ischemia, intracranial hemorrhages, CNS infection, and developmental brain anomalies.
Mechanisms of Epilepsy Genesis and Spread (Ictogenesis)
Physiologically, it is difficult to assess whether one seizure is the same as another, and studying seizures ‘in action’ is very difficult due to the temporal-spatial resolution of conventional neurological techniques such as EEG, as well as the fact that seizures do not happen that frequently in normal circumstances.
There are indeed several pro-ictal (seizure favoring) periods during which seizures are more likely to occur including sleep deprivation and medication withdrawal.
Furthermore, certain forms of epilepsy, such as autosomal dominant nocturnal frontal love epilepsy (ADFNLE) occur only in non-REM sleep, suggesting the importance of brain states in the initiation of epileptic seizures.
Naturally, the brain goes through many periods of excitation-inhibition that is not balanced – but what leads to in ictal imbalance? Episodic surges in network activity rarely cross a seizure threshold.
This is because positive feedback mechanisms including activity-dependent disinhibition are the normal functional mechanism to regulate such surges. The summed inputs to an epileptic network may have rare surges of the intensity of input, where levels of input above a seizure threshold rapidly degrade inhibition leading to a vicious cycle of further increases to overall network activity leading to ictogenesis.
The actual mechanisms that lead to ictal surges are still poorly understood. Some studies have demonstrated that short-term synaptic plasticity leading to depression of inhibitory GABAergic synapses and/or depression of glutamatergic synapses on inhibitory neurons leading to the seizure-threshold favoring synaptic formation.
Normally, functional ion channels and receptors would compensate for such dramatic changes, but mutations in epilepsy (or acquired lesions in adulthood) would leave the system susceptible to an excitation/inhibition imbalance – due to dysfunctional autoregulation of excitation/inhibition allowing surges of activity to pass a seizure threshold.
The bottom line is that those that have epilepsy have brain circuitry wired in a way that makes the neural networks (system) more susceptible for excitation surges to pass a critical ictal threshold due to abnormal regulation mechanisms caused by genetic mutations in ion channels, receptor subunits and/or downstream signaling pathways (e.g. mTOR/PI3K pathway).
In healthy people, the overall neural system would (largely) not allow electrical surges to pass a seizure threshold in normal circumstances – unless acquired through infections, injury, or drug abuse, leading to a failure of neuronal homeostasis.
Treatment Strategies
The goal of any treatment strategy for epilepsy is to lower the risk or chance that they may occur – due to their random and spontaneous nature. Many anti-epileptic drugs (AEDs) work by inhibiting voltage-gated sodium channels including phenytoin, valproic acid, and lamotrigine.
Others work by targeting potassium channels such as retigabine, whereas others work to target T-type calcium channels such as ethosuximide. Gabapentin targets the α2δ subunit of a particular voltage-gated calcium channel to inhibit it. Gabapentin is also used as an analgesic to treat neuropathic pain where nociceptive neurons become overactive.
All seizure medications/AEDs have side effects including sleepiness as well as issues with tolerance and dependency in the long term. In most cases (60-70%) AEDs may be effective, but in other cases, AEDs may not have any efficacy at all.
In such cases, other options including switching to a ketogenic diet may be prescribed or performing lesionectomy surgery or stimulation therapy. As mentioned earlier, sleep deprivation is pro-ictal, thus sleep management may also be important to reduce the risk of seizures.
In summary, epileptic seizures can occur due to inherent changes to the brain’s overall regulation of excitation/inhibition, caused by genetic mutations to ion channels and synaptic receptor subunits, or acquired through infection, lesions, or drug abuse.
Enhanced excitation of the brain can lead to a seizure threshold being crossed leading to a period of the intense neural activity causing a seizure. Many anti-epileptic drugs work by targeting ion channels to reduce overall excitation thus reducing the risk of developing a seizure.
Further Reading
Last Updated: Apr 28, 2020