Parkinson’s disease (PD) is a neurodegenerative disorder characterized by problems with movement and muscle control. Common signs of PD are tremors, slowed movement, problems with balance, and difficulty walking.
Parkinson’s Disease Overview
What happens in Parkinson’s disease? In the brain, there is an area called the substantia nigra wherein nerve cells produce dopamine. This neurotransmitter, dopamine, carries messages around the brain and is responsible for movement and coordination. In PD, these dopamine-producing nerve cells deteriorate and die, leading to mobility problems.
The disease is progressive, which means that there are initial mild symptoms that may go unnoticed early on. However, symptoms worsen over time until movement problems become apparent.
There is no cure for Parkinson’s disease. However, understanding its causes can help scientists develop therapeutic approaches to prevent or slow down the progression of the illness.
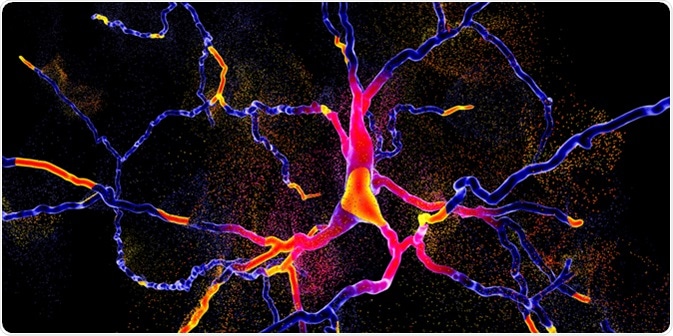
Degeneration of dopaminergic neuron, a key stage of development of Parkinson's disease, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
The Incidence of Parkinson’s Disease
Parkinson’s disease affects approximately one million people in the United States, with about 60,000 people diagnosed each year.
Worldwide, an estimated 10 million people live with Parkinson’s disease. However, the incidence may be higher, as many cases go undiagnosed until significant signs and symptoms of advanced disease appear.
Men have about a 50% increase risk of developing PD compared with women. For most patients, symptoms begin after the age of 50 years. However, about 5% of cases present as Young-onset Parkinson’s disease, between the ages of 21 and 40 years.
Causes and Risk Factors
A combination of hereditary, environmental, and genetic factors are thought to be associated with Parkinson’s disease. The disease manifestations reflect the low dopamine levels in the brain. However, the cause for these low levels is unknown.
Several factors may increase one’s risk of developing PD, including presence of certain genes and environmental triggers like pesticide or chemical exposure. Recently, the gut microbiome has been studied for a possible link to PD.
Gut Microbiome and Parkinson’s Disease
A well-balanced gut microbiome is crucial for maintaining general health. Alterations to the gut microbiome, which contains at least 1,000 species of bacteria and trillions of microorganisms, have been associated with many diseases.
.jpg)
Intestinal microbiome, bacteria colonizing different parts of digestive system, Bifidobacterium, Lactobacillus, Enterococcus and Escherichia coli, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
Many studies have focused on the possibility that the gut microbiome is connected to the development of Parkinson’s disease. Specifically, gut bacteria are thought to play a role in PD development.
One study, for instance, has shown that increased numbers of gut microbial taxa are found in the stools of patients with Parkinson’s disease compared with healthy controls.
Another study shows that PD symptoms are associated with the gut microbiome. Transplantation of fecal samples from patients with PD or healthy controls into healthy, germ-free mice showed that those receiving human microbiome samples from patients with PD then developed signs of PD. Receipt of samples from healthy persons did not trigger the development of PD symptoms.
Scientists at the University of Alabama found similar results in their study of 197 patients with PD and 130 healthy controls. Patients with PD had evidence of imbalanced gut microbiomes, in which some bacterial species existed in larger numbers and some in smaller numbers compared to healthy people.
These studies are just a few of the many exploring the connection between gut bacteria and Parkinson’s disease. Other investigations are also ongoing regarding possible connections between the gut microbiome at other neurologic diseases, such as dementia and autism.
Further Reading
Last Updated: Feb 27, 2019