New research highlights how GLP-1 receptor agonists influence gut bacteria, offering insights into their broader metabolic and anti-inflammatory benefits.
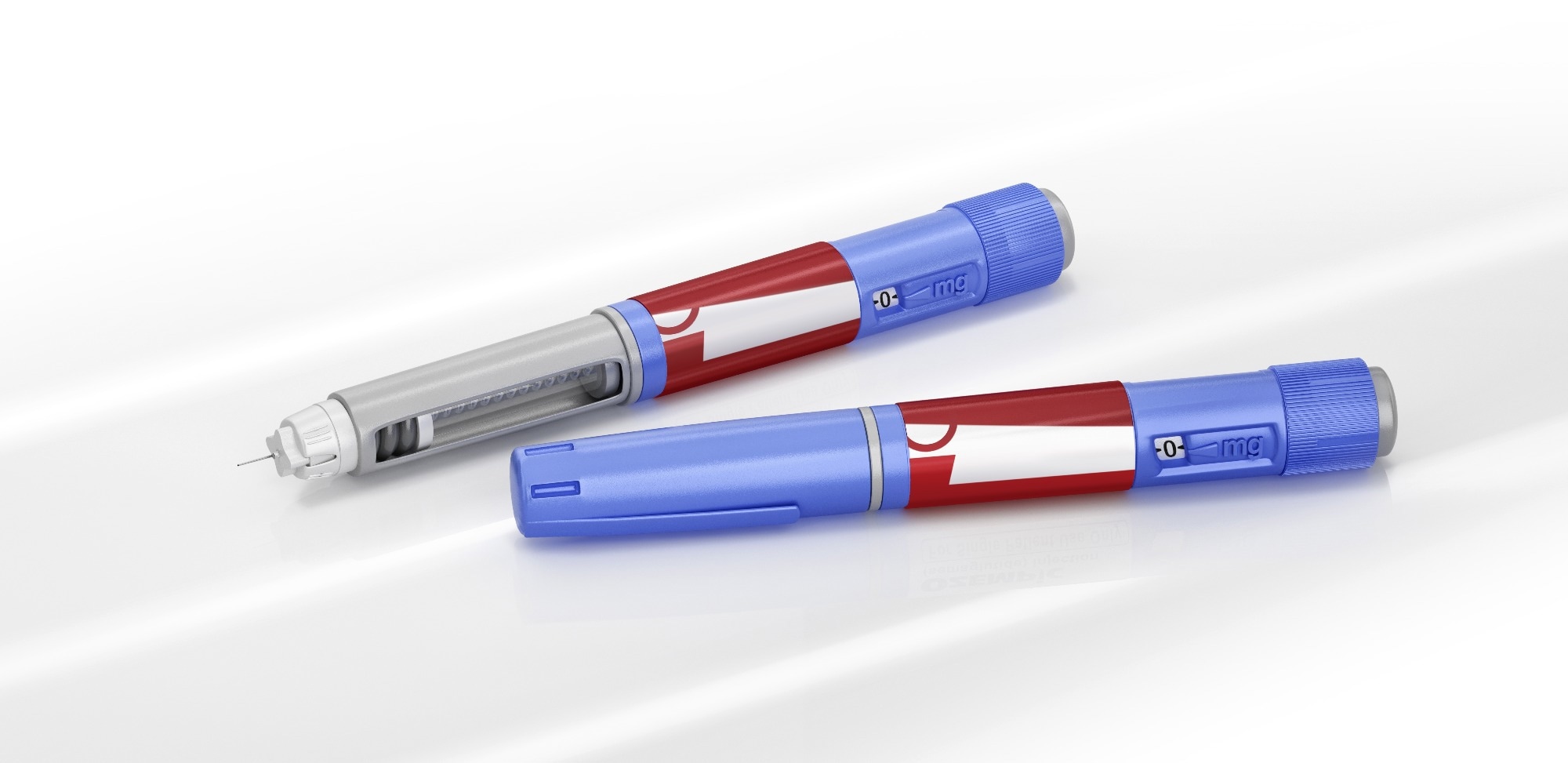 Study: Effects of GLP-1 Analogues and Agonists on the Gut Microbiota: A Systematic Review. Image Credit: Corona Borealis Studio/Shutterstock.com
Study: Effects of GLP-1 Analogues and Agonists on the Gut Microbiota: A Systematic Review. Image Credit: Corona Borealis Studio/Shutterstock.com
Glucagon-like peptide 1 (GLP-1) analogs and receptor agonists (GLP-1 RAs) are relatively new players in the medical landscape, but they’ve quickly gained attention for their effects on blood glucose, metabolism, weight loss, and even neurodegenerative diseases.
Now, researchers are turning their attention to another promising area: the gut microbiome. A recent review in Nutrients explores what we currently know about how GLP-1 RAs interact with gut microbes—and the broader implications for human health.
Introduction
GLP-1 is an incretin hormone that helps regulate blood glucose levels after meals, acting in a glucose-dependent manner. This means it lowers blood sugar without causing hypoglycemia—a key advantage in diabetes management.
Since its discovery in 1984 by Svetlana Mosjov, GLP-1 and its analogs (such as semaglutide, liraglutide, and dulaglutide) have rapidly become cornerstone treatments for type 2 diabetes mellitus (T2DM) and obesity. These drugs are effective in reducing blood sugar and promoting weight loss—two major risk factors for cardiometabolic disease—making them important tools for both prevention and treatment.
The American Diabetes Association (ADA) now recommends GLP-1 agonists for overweight individuals with diabetes, particularly those who experience frequent hypoglycemia with insulin or sulfonylureas.
Mechanistically, GLP-1 agonists enhance insulin secretion after meals, slow gastric emptying, and suppress glucagon release—all of which contribute to better glycemic control and weight management. These effects also appear to have a broader influence on metabolic health, potentially mediated through the gut microbiome.
Emerging evidence suggests that GLP-1 agonists support beneficial microbial growth, reduce inflammation in the gut, and may even help restore microbial balance disrupted by obesity and insulin resistance.
How GLP-1 affects the microbiome
GLP-1 RAs appear to shift the gut microbial ecosystem in favorable ways. For example, they reduce populations of Bacillota, a group of bacteria linked to obesity and insulin resistance, while also decreasing levels of Gram-negative bacteria that produce inflammatory compounds like lipopolysaccharides (LPS).
These changes could have systemic anti-inflammatory effects—benefitting not just metabolic health but possibly alleviating conditions like Crohn’s disease and ulcerative colitis.
T2DM itself is known to disrupt the gut microbiome, often leading to reduced diversity and a decline in beneficial genera like Bifidobacterium, Bacteroides, and Faecalibacterium, with increases in potentially harmful genera such as Ruminococcus, Fusobacterium, and Blautia.
The current review focused on how GLP-1 RAs—through their microbial effects—might influence the development and progression of T2DM.
Key findings from the review
The review analyzed 38 studies, most of which examined changes in the gut microbiome using fecal samples. Notably, 27 studies focused on liraglutide, while only 8 included human participants; the rest were conducted in animal models.
Liraglutide consistently promoted the growth of Akkermansia muciniphila, a microbe known to support gut barrier integrity and metabolic health. It also increased levels of Faecalibacterium prausnitzii, a key butyrate-producing bacterium with anti-inflammatory properties. At the same time, it reduced the prevalence of inflammation-associated microbes.
Exenatide and exendin-4 showed similar benefits in animal studies, enhancing populations of Akkermansia and Barnesiella, while suppressing bacteria linked to dysbiosis. In human studies, these agents increased levels of Coprococcus and Bifidobacterium, which are associated with improved metabolic outcomes and reduced inflammation.
Both liraglutide and exenatide also increased Lactobacillus reuteri, a beneficial microbe that enhances intestinal barrier function and promotes GLP-1 secretion.
Dulaglutide was less studied but showed promising signs in animals, increasing beneficial bacteria like Bacteroides, Akkermansia, and Ruminococcus. Human studies reported only minor shifts, with Lactobacillus being one notable increase.
Semaglutide produced mixed results in animal models. While it boosted A. muciniphila, it also appeared to reduce overall microbial diversity. These effects may depend on factors such as baseline metabolic status, dietary habits, and comorbid conditions.
Conclusions
This growing body of evidence suggests that GLP-1 analogs could influence the gut microbiome in ways that support long-term metabolic and intestinal health. As the review concludes, “The effect of GLP-1 analogues on the gut microbiota may have a positive impact on the long-term treatment of diabetes.”
However, further work is needed. Standardized study designs, consistent reporting methods, and better control of lifestyle and dietary variables are crucial to deepen our understanding of these interactions.
More robust human studies will be especially important to validate these findings and explore how microbial changes might affect patient outcomes over time.
Journal reference:
-
Gofron, K. K., Wasilewski, A., and Malgorzewicz, S., (2025). Effects of GLP-1 Analogues and Agonists on the Gut Microbiota: A Systematic Review. Nutrients. doi: https://doi.org/10.3390/nu17081303.