Teeth are one of the vital structures found in vertebrates helping in the mechanical breakdown of the food. Unlike other living organs, teeth possess a limited capacity to repair in case of injury or damage. For treating dental injuries, repair, restoration, and replacement of teeth are considered essential.

Image Credit: Josep Suria/Shutterstock.com
Tooth implantation using synthetic material, auto-transplantation, reshaping are some methods that are generally used for dental problems; however, the limitations associated with these techniques have urged researchers to explore alternate means.
The current progress in stem cell research has paved the way for promising avenues in the field of dental health. Scientists are exploring the possibilities of alternate regenerative medicine in repairing teeth by stem-cells therapy.
Dental stem cells can be an excellent source of autologous stem cells for pulp tissue restoration, lost periodontal ligament regeneration, and tooth structures generation (partial or complete) for biological implants.
Development of the tooth
Teeth formation involves the interaction of oral epithelium and mesenchyme. Oral epithelium originates from ectoderm, while mesenchyme originates from the neural crest. The tooth contains two specialized hard tissues - dentin and enamel - attached to the periodontal ligament.
Oral epithelium gives rise to dental enamel, whereas mesenchymal cells form cementum, dentin pulp, and periodontal ligaments. In addition to this, progenitor cells from mesodermal cells and neural crest cells give rise to craniofacial bones – the bones of the skull and face.
Oral epithelium thickening is the initial step in the development of teeth and leads to the formation of the dental lamina on the lingual side (near the tongue) and vestibular lamina on the vestibular side (near the inner ear).
While the dental lamina gives rise to the teeth, the vestibular lamina creates a deep furrow or groove (sulcus) between the cheek and the teeth.
The next step is the proliferation of the dental lamina to form placodes. The placodes invade the mesenchyme and form the tooth bud. The tooth bud formation is followed by controlled cell growth and differentiation, which leads to the formation of the tooth crown.
Now, the mesenchymal cells form dental papilla, which differentiates into cells that form dentin and enamel. The evolution and development of the teeth continue postnatally, making the outer covering of the enamel harder; subsequently, the root of the teeth develops, and teeth erupt in the oral cavity.
Stem cells in teeth repair
Stem cells are an excellent treatment option for dental injuries and various dental conditions. The tooth provides highly proliferative stem cells, which can be used for dental or non-dental purposes and these stem cell-based therapies can be used to treat life-threatening diseases.
Dental stem cells can be easily obtained from teeth that are naturally lost or surgically removed. These tissues can be isolated from pulp of both exfoliated (in kids) and adult teeth, from the periodontal ligament linking the tooth root with the bone, from the tips of developing roots and from the tissue that adjoins the unerupted tooth.
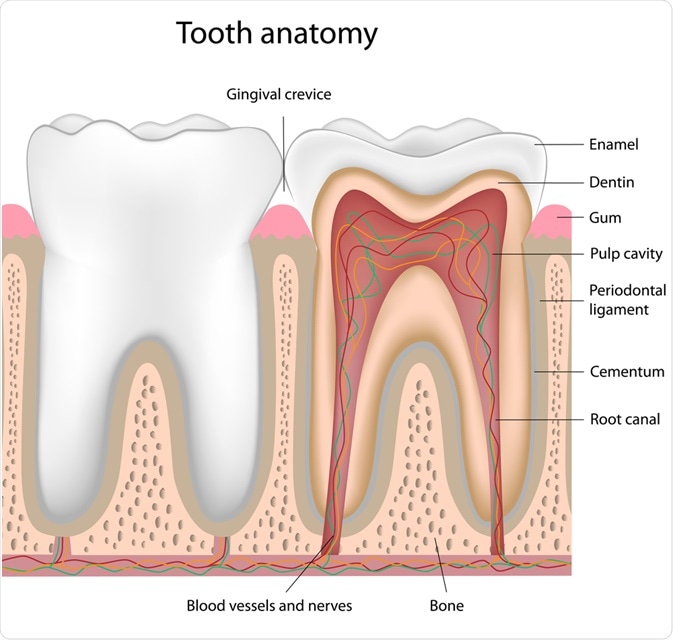
Image Credit: Alila Medical Media/Shutterstock.com
The following are some dental stem cells that have been isolated and characterized:
Dental Pulp Stem Cells
Dental pulp stem cells are a source of cells to facilitate and repair damaged cells. These cells were first isolated from permanent third molar of adult humans.
They have the capability of differentiating in vitro into mesenchymal cell derivatives such as odontoblasts, adipocytes, chondrocytes, and osteoblasts.
Stem cells from human exfoliated deciduous teeth
Stem cells isolated from the pulp of human exfoliated deciduous teeth (SHED) have the capability of producing dentine and inducing bone formation. SHED has a higher rate of proliferation that the dental pulp stem cells and are reported to double the population of the cells.
SHED is a useful tool in dental pulp tissue engineering – a procedure in which the pulp is removed and replaced with stem cells. Studies demonstrate that the tissues formed via tissue engineering using SHED resemble natural dental pulp structurally and histologically.
Periodontal ligament stem cells
Periodontal ligament stem cells are fibrous connective tissue comprising of specialized cells between the cementum and inner walls of alveolar bone.
Periodontal ligament stem cells include progenitor cells capable of differentiating into cementoblast-like cells, connective tissue, and adipocytes rich in collagen. Periodontal ligament stem cells are proposed to be effective in periodontitis, a gum disease that involves infection and inflammation.
Root apical papilla stem cells
Stem cells from the root apical papilla are located at the tips of growing tooth roots and are only present during root development before the eruption of the tooth. These cells can differentiate into odontoblasts and adipocytes.
Dental follicle stem cells
Dental follicle cells include a group of mesenchymal progenitor cells enclosing the tooth germ - a group of cells that eventually forms a tooth.
Dental follicle cells are responsible for the formation of cementum, periodontal ligament, and alveolar bone during tooth development.
Clinical Implications
Periodontitis
In periodontitis, there is an irreversible loss of connective tissue attachment and the supporting bone. To regenerate periodontium, researchers have used different populations of dental stem cells to replicate vital events in periodontal development.
As per a study by Honda et al, published in the journal Cells Tissues Organs, implantation of engineered cells, derived from periodontal ligament stem cells, can facilitate transplantation of periodontal cells.
Regeneration of Dental Pulp
In case of severe infection, the dental pulp is removed and treated by the restoration of the tooth pulp with the help of cement. This procedure results in the death of the tooth. In a study by Huang et al, dental stem cells were able to regenerate dental pulp in emptied root canal space.
The researchers used stem cells from dental pulp and root apical papilla. The stem cells were isolated from the third human molar and transplanted into mice.
After 3-4 months, the root canal space was found to be filled with well-established vascularization. Additionally, the continuous layer of tissues resembling dentine was deposited on the dentinal walls of the canal.
Whole tooth regeneration
Currently, the treatment for complete tooth regeneration involves screwing metal rod in the bone and capping it with plastic or ceramic crown.
The use of tooth implants is an option; however, implant use is challenging - the implants are connected directly to the bone, and thus the force of chewing is directly transmitted to the bone in the absence of periodontal ligament, which acts as a shock absorber.
In cases where bones are insufficient, bone grafting needs to be done before the implantation.
Stem cells can be used in tooth regeneration, which could help personalize dental treatment to a great extent and avoid the challenges found with current treatment options.
To conclude, dental stem cells are showing a promising future in treating teeth injuries and damage. Still, its success in therapeutic use will not only depend on ease of administration but also the efficiency and quality of repair concerning cost.
Sources
- Honda M.J., et al. (2009). Enamel tissue engineering using subcultured enamel organ epithelial cells in combination with dental pulp cells. Cells Tissues Organs;189:261–267. doi: 10.1159/000151743.
- Huang., et al (2010). Stem/progenitor cell-mediated de novo regeneration of dental pulp with a newly deposited continuous layer of dentin in an in vivo model. Tissue engineering. Part A, 16(2), 605–615. doi.org/10.1089/ten.TEA.2009.0518
- Sakai V.T., et al. (2010). SHED differentiate into functional odontoblasts and endothelium. J. Dent. Res;89:791–796. doi: 10.1177/0022034510368647
- Wang, J., et al. (2010). Stem cells from human-exfoliated deciduous teeth can differentiate into dopaminergic neuron-like cells. Stem cells and development, 19(9), 1375–1383. doi.org/10.1089/scd.2009.0258
- Mozaffari, M. S., et al. (2019). Stem cells and tooth regeneration: prospects for personalized dentistry. The EPMA Journal, 10(1), 31–42. https://doi.org/10.1007/s13167-018-0156-4
Further Reading
Last Updated: Apr 30, 2020