2024 update
Which SARS-CoV-2 lineages are classified as VOC or VOI now?
How do RNA viruses mutate?
B.1.1.7 lineage (Alpha variant)
B.1.351 lineage (Beta variant)
P.1 lineage (Gamma variant)
B.1.427/B.1.429 lineage CAL.20C variant (Epsilon variants)
B.1.525 (Eta variant) and B1.526 (Iota variant) lineages
B.1.617 lineage (Kappa and Delta variants)
B.1.1.529 lineage (Omicron variant)
P.2 lineage (Zeta variant)
Mutations of concern
D614G
N501Y
E484K or “Eek”
E484Q
K417
L452R
Q677
P681H
S943P
V483a
S477G/N
Which regions of the SARS-CoV-2 genome mutate the most?
Which SARS-CoV-2 variants have been found?
Current ECDC Classification of SARS-CoV-2 Variants
References
2024 Update
As of December 2023, most or all measures against COVID-19 have been relaxed around the world, in large part owing to the great success of the various vaccines developed during and after the pandemic. The SARS-CoV-2 virus is still circulating strongly, however, and novel strains are constantly emerging as others die away. According to the CDC, between the dates of 10th December to 16th December 2023, 25,577 individuals were hospitalized with COVID-19 in the USA, a 10.4% rise on the previous week. Currently, no variant of SARS-CoV-2 is considered a variant of concern (VOC) by the Centers for Disease Control and Prevention (CDC) in the USA or the European Center for Disease Prevention and Control (ECDC).
The CDC defines a VOC as a strain with increased transmissibility, more severe disease symptoms, reduced neutralization by antibodies generated by previous infection or vaccination, and/or reduced effectiveness of established treatments or diagnostic procedures. A variant of interest (VOI) is a strain exhibiting reduced neutralization by antibodies, efficacy of treatment or diagnostic tests, and/or possessing a predicted but not demonstrated increase in transmissibility or disease severity. Finally, the CDC also categorizes some strains as variants being monitored (VBM), which are those with known genetic sequences with the potential to impact existing medical countermeasures, either because previous strains exhibited this capacity or they possess a large number of antigenic mutations with a large presence in multiple countries. A furthermore severe classification is that of a variant of high consequence (VOHC), which presents a much more serious clinical disease and reduced susceptibility to treatment. No variants are currently classified as VOHC.
Which SARS-CoV-2 lineages are classified as VOC or VOI now?
Most recently, on 1st September 2023, the CDC classified variants of SARS-CoV-2 carrying the F456L mutation to the spike protein as VOI. This mutation is recognized by the ECDC as a lineage in the Omicron variant (XBB.1.5-like), with dominant transmission in the EU and USA, though it is stated to have only a baseline impact on immunity and disease severity. Other spike mutations of interest within this lineage listed by the ECDC include N460K, S486P, and F490S. The ECDC also maintains two other lineages of the Omicron variant as VOI: BA.2.75 and BA.2.86. Two lineages are considered variants under monitoring by the ECDC, equivalent to the CDCs VBM: XBB.1.5-like and DV.7.1.
A large number of SARS-CoV-2 variants have been de-escalated by the ECDC either because they are no longer circulating, the variant has been circulating for a long time with little impact on the overall epidemiological situation, or scientific evidence has demonstrated that the variant poses no concerning properties. This includes the early VOC alpha lineage (B.1.1.7), which largely declined during the emergence of the Delta variant (B.1.617.2), which itself then gradually declined to inconsequential levels as other lineages emerged, namely Omicron.
According to a severity assessment of various historic and currently circulating SARS-CoV-2 variants by Nyberg et al. (2023) the Omicron variant poses 59% lower risk of hospitalization than the Delta variant did, with 88% lower risk of intensive care unit admission, and 69% lower chance of death. This is particularly pronounced in adults, while children already possessed a relatively low risk. When separating the vaccinated (two doses, no booster) from the unvaccinated, the former see a 33-49% lower chance of hospitalization from Omicron compared with Delta, while the unvaccinated or those who had received two vaccinations and boosters see a larger 70% lesser chance. This is consistent with waning vaccine effectiveness towards Omicron BA.1 without boosters, and indicative of the lower severity of this variant.
The below article was first published in 2021 and has been updated regularly. The information below serves as a record of how the variants of concern evolved over the course of the pandemic.
How do RNA viruses mutate?
The mutation rate of single-stranded ribonucleic acid (ssRNA) viruses is observed to be much higher than organisms that possess single-stranded deoxyribonucleic acid (ssDNA), and many times more than those with double-stranded DNA (dsDNA). Not all mutations necessarily increase virulence and, in the majority of cases, may in fact be deleterious or inconsequential.
Therefore, organisms must find an equilibrium between a high mutation rate that allows them to adapt to changing environmental conditions, and a low one that lessens the incidence of catastrophic mutations. Small DNA viruses may encode their own DNA repair, and some RNA viruses also share the ability to check for and repair replication errors.
However, while DNA viruses generally rely on the transcription machinery of the host cell, RNA viruses encode for their own transcription machinery. This means that the replication and mutation rate of RNA viruses is more directly related to their own genome and is thus subject to the same evolutionary pressures.
Vignuzzi & Andino (2012) note that the offspring of RNA viruses, with genomes commonly falling into the size range of 7-12 kilobases (kb) in length, tend to bear one or two distinct mutations per nucleotide site. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) genome is thought to be around 27-31 kb in length, which increases the overall number of mutations acquired, without necessarily increasing the incidence rate.
The ability to rapidly acquire new genetic characteristics allows viruses to emerge in novel hosts, avoid vaccine-induced immunity, and become more virulent. Moreover, this ability can also be a double-edged sword in terms of improving overall genome fitness.
The World Health Organization (WHO) recently announced a nomenclature system for naming and tracking SARS-CoV-2 that will assist in the public discussions of variants as they emerge. This nomenclature system was developed by virological, microbial, nomenclature, and communication specialists from around the world to ensure that the SARS-CoV-2 variants are easy to pronounce and avoid any potentially stigmatizing terms. To this end, the expert group convened by WHO has recommended using letters of the Greek alphabet as names for each new SARS-CoV-2 variant.
How Viruses Like The Coronavirus Mutate
B.1.1.7 lineage (Alpha variant)
One new strain with a particularly large number of mutations was first noted in the United Kingdom in September 2020, termed VOC 202012/01 (a variant of concern – December 2020). The B.1.1.7 variant is also known as 20B/501Y.V1 by the United States Centers for Disease Control and Prevention (CDC), as well as the Alpha variant according to the WHO. This strain, which has since been termed the B.1.1.7 variant, has a total of 23 mutations with 17 amino acid changes.
Since its identification in Britain, the B.1.1.7 strain has been found in over 90 different countries around the world. In fact, as of April 7, 2021, the B.1.1.7 variant is the most common source of new SARS-CoV-2 infections in the United States.
What is concerning about this specific strain is that it is thought to be 30-50% more infectious than the original SARS-CoV-2 strains and may be more deadly. However current vaccines still work on the strain.
The B.1.1.7 strain has the following key mutations:
- N501Y
- P681H
- H69-V70 and Y144/145 deletions
SARS-CoV-2 interacts with ACE2 receptors in the body using its spike protein. This consists of two subunits, the first of which contains the receptor-binding domain. The B.1.1.7 lineage has a mutation on the receptor-binding domain, specifically with an asparagine amino acid being replaced with tyrosine at position 501, thus the mutation is termed N501Y.
Additionally, the strain often shows a deletion of amino acids 69 and 70, also seen to arise spontaneously in other strains, causing a conformational change of the spike protein.
At position 681, a mutation from a proline amino acid to histidine has also been found to arise spontaneously in several strains and is prominent in B.1.1.7, as is a mutation to open reading frame 8, the function of which is not yet fully understood.
Evidence suggests that this strain is more transmissible, though it does not appear to lessen vaccine efficacy. Recent studies suggest this strain is more deadly, linked to a higher chance of hospitalization.
B.1.351 lineage (Beta variant)
Another strain, B.1.351 also shares the N501Y mutation. The B.1.351 strain is also known as 20C/501Y.V2 or the Beta variant. The Beta SARS-CoV-2 variant was first detected in South Africa in October of 2020 and has since been found in more than 48 other countries since then.
The B.1.351 strain has the following key mutations:
This South African variant is believed to be about 50% more transmissible as compared to previous variants that have been identified in South Africa. To date, the Pfizer-BioNTech vaccine has been found to be 75% effective against infection by this variant. Furthermore, vaccine effectiveness against severe, critical, or fatal disease due to SARS-CoV-2 infection with this variant, as well as the B.1.1.7 variant, has been found to be 97.4%.
Unfortunately, the University of Oxford-AstraZeneca vaccine has been found to be less effective against the B.1.351 variant, which has led South Africa to suspend the national roll-out of this specific vaccine.
P.1 lineage (Gamma variant)
The P.1 lineage of SARS-CoV-2, which is also known as 20J/501Y.V3 or the Gamma SARS-CoV-2 variant, was first described in Japan by the National Institute of Infectious Diseases, thought to have arrived in the country from Brazil on the 6th of January. The variant has been traced back to Manaus, Brazil.
The strain is not thought to be more deadly but is more transmissible than the original strain of SARS-CoV-2.
The P.1 strain has the following key mutations:
The P.1 lineage is a branch of the B.1.1.248 lineage and bears 12 mutations in the spike protein, including the previously mentioned N501Y and an exchange of glutamic acid with lysine at position 484 (E484K). It is a close relative of the B.1.351 strain.
The E484K mutation had previously been reported in a different lineage originating in Brazil as early as the summer of 2020 (B.1.1.28).
Clinical trial data using the Moderna mRNA vaccine has found that a single booster shot of this vaccine successfully increased neutralizing titers against the virus and the B.1.351 and P.1 variants in individuals who were previously vaccinated. Notably, this booster shot involved the use of the mRNA-1273.351 vaccine, which is a strain-matched vaccine that has been derived from the original Moderna mRNA vaccine denoted as mRNA-1273.

Image Credit: thodonal88/Shutterstock.com
B.1.427/B.1.429 lineage CAL.20C variant (Epsilon variants)
The CAL.20C variant which spans the B.1.427 and B.1.429 lineages is believed to have emerged in California in May of 2020. Both of these variants, which are collectively termed as the Epsilon variants, are believed to be 20% more infectious than preexisting variants strains although does not seem to be spreading as fast as some variants like the B.1.1.7.
The B.1.427/B.1.429 variants have now been detected in North America, Europe, Asia and Australia. Researchers have found that neutralizing antibodies obtained from people who had previously received either the Moderna or Novavax vaccinations were slightly less effective against these variants, but still generated effective protection. Although the Pfizer vaccine was not studied in this paper, researchers believe that since it uses a similar technology to that which is incorporated into the Moderna vaccine, that it would likely have a similar response.
This strain has the following key mutations:
B.1.525 (Eta variant) and B1.526 (Iota variant) lineages
In December of 2020, the B.1.525 variant, which is otherwise known as the Eta variant, was first found to be spreading throughout New York City. Like the B.1.1.7 lineage of SARS-CoV-2 variants, the B.1.525 variant also appears to have the same E484K mutation and the H69-V70 deletion. In addition to these mutations, the B.1.525 variant lineage also carries the Q677H mutation.
In addition to the B.1.525 lineage, the B.1.526 lineage of variants, otherwise known as the Iota variants, have also been identified in New York City. Notably, the B.1.526 lineage appears in two forms; one with the E484K spike mutation, whereas the other form of this variant has the S477N mutation.
It appears that neutralizing antibodies from both the convalescent plasma of patients who have recovered from COVID-19, as well as those which are produced post-vaccination are less effective against these two variants; however, further work must be conducted to confirm this observation.
B.1.617 lineage (Kappa and Delta variants)
The B.1.617 strain has been dubbed the “double mutant virus” due to two of the concerning mutations it carries. These two key mutations are:
The rapid rate at which this variant has spread across India indicates to some scientists that this variant is highly transmissible. This observation is largely due to the fact that the B.1.617 variant appears to have a greater prevalence as compared to the other variants that have been detected in India, such as the B.1.618 variant that was originally present in West Bengal.
As the B.1.617 variant continues to spread at an alarming rate in India, three different subtypes of this variant have been identified which include B.1.617.1, B.1.617.2, and the B.1.617.3 variants. As compared to the first subtype of this variant, which is also known as the Kappa variant, data suggests that the B.1.617.2 or Delta variant has a growth rate advantage that has allowed for it to become the dominant subtype found in much of India.
To date, it is not yet fully understood what makes the B.1.617.2 variant so transmissible and whether current vaccines can offer protection against this variant. However, one study produced by a team of researchers at the University of Cambridge found that the neutralizing antibodies generated by individuals who were previously vaccinated with one dose of the Pfizer vaccine are about 80% less potent against some B.1.617 mutants.
Furthermore, a team of German researchers also found that neutralizing antibodies collected from patients who were previously infected by SARS-CoV-2 were 50% less effective at neutralizing these circulating strains. It should be noted, however, that this data does not necessarily indicate that the vaccines are ineffective against these variants.
B.1.1.529 lineage (Omicron variant)
On November 24, 2021, South Africa reported a new SARS-CoV-2 variant that was named by the WHO as B.1.1.529, or the Omicron variant. This variant was first identified in samples that were collected on November 11, 2021 in Botswana and on November 14, 2021 in South Africa.
Since its initial identification, the Omicron variant has been in several other countries around the world including Brazil, Australia, Saudi Arabia, England, Spain, France, Denmark, the Netherlands, Germany, Italy, Japan, South Korea, Canada, and the United States. In fact, as of December 6, 2021, over a third of the states in the United States have already detected COVID-19 cases that were positive for the Omicron variant. Despite its widespread detection in the United States, it should be noted that the Delta variant remains the dominant variant responsible for about 99.9% of new COVID-19 cases.
Soon after its detection, the WHO classified the Omicron variant as a VOC based on epidemiological data that indicated a rise in SARS-CoV-2 infections that coincided with the detection of this variant. Furthermore, the Omicron variant has numerous protein substitutions within the spike protein, some of which have already been detected in other SARS-CoV-2 variant and are associated with reduced susceptibility to neutralization by both monoclonal antibody therapies, as well as convalescent and vaccinee sera.
As previously mentioned, the Omicron variant has several key amino acid substitutions present within the SARS-CoV-2 spike protein. These include A67V, del69-70, T951, de142-144, Y145D, del211, L212I, ins214EPE, T547K, D614G, H655Y, N679K, P681H, N764K, D796Y, N856K, Q954H, N969K, and L981F. More specifically, within the receptor binding domain (RBD) of this variant are several additional mutations, of which include G339D, S371L, S373P, S375F, K417N, N440K, G446S, S477N, T478K, E484A, Q493R, G496S, Q498R, N501Y, and Y505H. Taken together, the Omicron variant contains several additional changes to the spike protein that have not been observed in other variants of SARS-CoV-2, 15 of which have been identified in the RBD.
Although several of the mutations in the Omicron variant have already been reported in other SARS-CoV-2 variants, the combination of so many different substitutions may not necessarily create a more dangerous strain of SARS-CoV-2. For example, although the Omicron variant has both the N501Y and Q498R mutations, both of which are associated with increased binding affinity to the ACE2 receptor, the presence of other protein substitutions in the spike protein of this variant may instead decrease binding to ACE2.
The Omicron variant comprises a number of lineages and sublineages, i.e., BA.1, BA1.1, BA.2, BA.2.75, BA.3, BA.4, BA.5, and XAK. Nevertheless, the three most common lineages are BA.2, BA.4, and BA.5. The CDC stated that individuals can transmit the virus onto others, irrespective of their vaccination status and/or prevalence of symptoms. The transmission rate of Omicron variants is higher than the Delta strain. Importantly, Omicron has been seen to re-infect individuals who have recently recovered from COVID-19.
Individuals infected with the Omicron variant displayed symptoms similar to previous variants. The majority of these individuals presented mild symptoms; however, some required hospitalization. The severity of the infection mostly depended on the vaccination status.
The current COVID-19 vaccines provide protection against severe illness and deaths due to infection with the Omicron variant. Nevertheless, breakthrough infection among the vaccinated population has been reported. Scientists are currently working to determine the optimal COVID-19 treatment. Among the available monoclonal antibodies’ treatment, some have been found to be less effective against particular Omicron strains than others.
Presently, the U.S. CDC and other national agencies have also recommended that the public continues to use all currently available prevention strategies to reduce the spread of this variant including masking, improved ventilation systems, social distancing, handwashing, and periodic testing for SARS-CoV-2 infections.
P.2 lineage (Zeta variant)
The P.2 lineage of SARS-CoV-2 variants, which are otherwise known as the Zeta variants, independently accrued the spike E484 mutation and was originally identified in Brazil in April 2020. To date, there is limited information on whether monoclonal antibody therapies and the antibodies generated post-vaccination have reduced efficacy against this variant of concern.

Image Credit: PX Media/Shutterstock.com
Mutations of concern
The apparent spontaneity of the development of some of the key mutations that have been discussed here suggests that the virus could be experiencing convergent selection pressures around the globe, with the most transmissible forms outcompeting their cousins.
The current mutations of concern that may be aiding the spread of coronavirus include:
D614G
The D614G mutation is of B.1 lineage and appeared in early 2020. This mutation quickly spread across the world and became dominant.
The D614G mutation is a missense mutation in which an altered single DNA base pair causes the substitution of aspartic acid (single-letter code: D) with glycine (single-letter code: G) in the protein that the mutated gene encodes.
N501Y
This mutation is present in several lineages including B.1.345, B.1.17, P.1, and B.1.1.529 variants. This mutation changes the amino acid asparagine (N) to tyrosine (Y) at position 501 in the RBD of the spike protein, which may allow SARS-CoV-2 strains with this mutation to have a greater binding affinity to the ACE2 receptor on host cells.
E484K or “Eek”
This spike protein mutation has been found in several lineages and may aid the virus in avoiding some antibody types. In it, there is an exchange of glutamic acid with lysine at position 484.
E484Q
This spike protein mutation is also mutated at position 484, with the exception that the glutamic acid is substituted with glutamine. This mutation is thought to increase immune evasion and ACE2 binding.
K417
This spike protein mutation has been found in several lineages, including P.1 and B.1.351. It is also thought to help the virus bind to cells more tightly.
This mutation is K417N in the B.1.351 and B.1.1.529 strains, and K417T in the P.1 strain.
L452R
The L452R spike protein mutation has appeared in several lineages. In this mutation, there is a leucine to arginine substitution at amino acid 452. The mutation is thought to increase immune evasion and ACE2 binding.
This mutation was observed in both the U.S. and Europe in 2020, before increasing in prevalence in January 2021, as it is notably present in the CAL.20C variant that has become widespread in California, particularly in Los Angeles. It is also notably present in the B.1.617 variant.
Notably, laboratory studies have found that specific monoclonal antibody treatments may not be as effective in treating COVID-19 caused by variants with the L452R or E484K mutations.
Q677
The Q677 mutation is located on the side of the SARS-CoV-2 spike protein, thereby suggesting that it may play a role in increasing the penetrability of the virus into human cells. To date, the Q777 mutation has been identified in several different SARS-CoV-2 variant lineages, seven of which have been identified in the United States. The Q677 variant has not yet been determined to be more infectious as compared to preexisting mutations.
P681H
The P681H mutation is found in the B.1.1.7 and B.1.1.529 strains, with a different variation of this mutation (P681R) found in the B.1.617.2 variant. The presence of this mutation has been shown to increase spike cleavage, which could allow for increased transmissibility of affected strains.
S943P
The S943P mutation was first found in the SARS-CoV-2 spike protein in Belgium. This mutation is a result of recombination of different viruses in an infected host.
V483a
The V483a mutation occurred in the receptor binding motif (RMB) of S1 domain of the spike protein of SARS-CoV-2. This mutation is involved with the replacement of hydrophobic valine by hydrophobic alanine, at position 483.
S477G/N
The S477 mutation occurs due to changes in amino acids at position 477. This mutation is predominantly found in the receptor binding domain of the spike protein. S477G and S477N are mainly responsible for the enhancement of the binding affinity for hACE2. The Omicron variant contains S477G and S477N mutations.
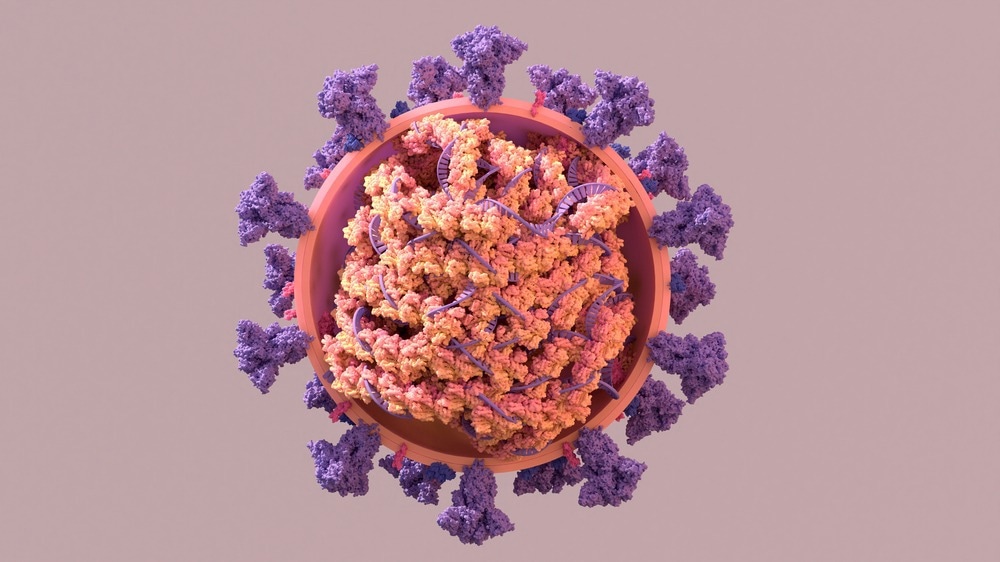
Image Credit: Design_Cells/Shutterstock.com
Which regions of the SARS-CoV-2 genome mutate the most?
A large meta-study performed by Koyama, Platt & Parida (2020) gathered over 10,000 SARS-CoV-2 genomes worldwide and compared them to detect the most common mutations, identifying nearly 6,000 distinct variants.
The most divergent genome segment was ORF1ab, which is the largest by far as it occupies around a third of the genome. ORF1ab is transcribed into a multiprotein complex that is eventually cleaved into a number of nonstructural proteins that are involved in transcription. Some of these proteins are the target of anti-viral drugs remdesivir and favipiravir, which may be a cause for concern regarding the development of a strain against which these drugs have no effect.
The second most diverse region of the SARS-CoV-2 genome is around the spike protein, which must remain largely conserved in order to interact with ACE2. Some mutations, such as D364Y, have been reported to enhance the structural stability of the spike protein, increasing its affinity for the receptor. However, most are likely to lessen the virulence of the virus to such an extent that the lineage quickly dies off.
Which SARS-CoV-2 variants have been found?
Recently, the European Center for Disease Prevention and Control (ECDC) has presented the list of SARS-CoV-2 variants, categorized into variants of concern (VOC), variants of interest (VOI), variants under monitoring (VUM), and de-escalated variants. The categorization of SARS-CoV-2 variants is based on available genomic epidemiological and in vitro evidence.
SARS-CoV-2 variants categorized under VOC have significant impact on disease severity, transmissibility, and evasion of immune responses. These variants significantly affect the epidemiological situation in the European Union. Although VOIs strongly possess the potential to cause adverse epidemiological situation, the supporting evidence is at the infancy stage and has major uncertainties.
Based on genomic variant screening and preliminary scientific evidence, VUM mutants carry some properties similar to VOCs. Nevertheless, the evidence is either not robust enough for assessment or has not yet been evaluated by ECDC. These variants are currently being vigilantly monitored.
De-escalated variants are those which satisfy at least one of the following criteria:
(a) Variants that have been circulating for a prolonged period without affecting the overall epidemiological situation.
(b) Variants that are no longer circulating.
(c) Scientific evidence strongly suggesting the absence of any concerning properties.
Current ECDC Classification of SARS-CoV-2 Variants
|
Variants of Concern
|
|
Name
|
Lineage
|
Year and Month First Detected
|
Location of Emergence/Prevalence
|
|
Omicron
|
BA.1
|
November 2021
|
South Africa and Botswana
|
|
Omicron
|
BA.2
|
November 2021
|
South Africa
|
|
Omicron
|
BA.4
|
January 2022
|
South Africa
|
|
Omicron
|
BA.5
|
January 2022
|
South Africa
|
|
Variants of Interest
|
|
Name
|
Lineage
|
Year and Month First Detected
|
Location of Emergence/Prevalence
|
|
Omicron
|
BA.2+L452X
|
-
|
-
|
|
Omicron
|
BA.2.75
|
May 2022
|
India
|
|
Variants under Monitoring
|
|
Name
|
Lineage
|
Year and Month First Detected
|
Location of Emergence/Prevalence
|
|
Omicron
|
BA.3
|
November 2021
|
South Africa
|
|
Omicron
|
XAK
|
June 2022
|
Germany
|
|
De-escalated Variants
|
|
Name
|
Lineage
|
Year and Month First Detected
|
Location of Emergence/Prevalence
|
| Alpha |
B.1.1.7 |
September 2020 |
United Kingdom |
| Epsilon |
B.1.427/B.1.429 |
May 2020 |
United States of America |
| Eta |
B.1.525 |
December 2020 |
Nigeria |
| Theta |
P.3 |
January 2021 |
The Philippines |
| Kappa |
B.1.617.1 |
December 2020 |
India |
| Iota |
B.1.526 |
December 2020 |
United States of America |
| Zeta |
P.2 |
January 2021 |
Brazil |
| Lambda |
C.37 |
Decemeber 2020 |
Peru |
| Beta |
B.1.351 |
September 2020 |
South Africa |
| Gamma |
P.1 |
December 2020 |
Brazil |
| Delta |
B.1.617.2 |
December 2020 |
India |
Article last updated on 12th August 2022 by Dr. Priyom Bose.
References
- SARS-CoV-2 variants of concern as of 4 August 2022. The European Center for Disease Prevention and Control (ECDC). https://www.ecdc.europa.eu/en/covid-19/variants-concern
- Aleem, A., Akbar Samad A.B., and Slenker, A.K. (2022) Emerging Variants of SARS-CoV-2 And Novel Therapeutics Against Coronavirus (COVID-19). In StatPearls. StatPearls Publishing. https://pubmed.ncbi.nlm.nih.gov/34033342/
- Arora S. (2022). Omicron: A variant of concern not a cause of panic. Journal of Advanced Pharmaceutical Technology & Research, 13(2), pp.138–140. https://doi.org/10.4103/japtr.japtr_14_22
- Brief report: New Variant Strain of SARS-CoV-2 Identified in Travelers from Brazil (2021) National Institute of Infectious Diseases. https://www.niid.go.jp/niid/en/2019-ncov-e/10108-covid19-33-en.html
- Duffy, S. (2018) Why are RNA virus mutation rates so damn high? PLoS Biology, 16(8). https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000003
- Emerging SARS-CoV-2 Variants (2021) Centers for Disease Control and Prevention. https://www.cdc.gov/
- Koyama, T., Platt, D. & Parida, L. (2020) Variant analysis of SARS-CoV-2 genomes. Bulletin World Health Organization, 98(7). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7375210
- Number of total and positive coronavirus (COVID-19) tests conducted in the U.S. as of January 11, 2021, by state (2021) Statistica. https://www.statista.com/statistics/1111716/covid19-us-positive-tests-by-state/
- Pereira, F. (2020) Evolutionary dynamics of the SARS-CoV-2 ORF8 accessory gene. Infection, Genetics and Evolution, 85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7467077/
- The New York Times. 2021. Coronavirus Variants and Mutations [online] Available at https://www.nytimes.com/interactive/2021/health/coronavirus-variant-tracker.html [Accessed 22 March 2020]
- Vignuzzi, M. & Andino, R. (2012) Closing the gap: the challenges in converging theoretical, computational, experimental and real-life studies in virus evolution. Current Opinion in Virology, 2(5). https://www.sciencedirect.com/science/article/pii/S1879625712001435?via=ihub
- Abu-Raddad, L.J., Chemaitelly, H. and Butt, A.A. (2021). Effectiveness of the BNT162b2 Covid-19 Vaccine against the B.1.1.7 and B.1.351 Variants. New England Journal of Medicine.
- investors.modernatx.com. (n.d.). Moderna Announces Positive Initial Booster Data Against SARS-CoV-2 Variants of Concern | Moderna, Inc. [online] Available at: https://investors.modernatx.com/overview/default.aspx
- Abdool Karim, S.S. and de Oliveira, T. (2021). New SARS-CoV-2 Variants — Clinical, Public Health, and Vaccine Implications. New England Journal of Medicine.
- Vaidyanathan, G. (2021). Coronavirus variants are spreading in India — what scientists know so far. Nature. [online] Available at: https://www.nature.com/articles/d41586-021-01274-7.
- Facebook, Twitter, options, S. more sharing, Facebook, Twitter, LinkedIn, Email, URLCopied!, C.L. and Print (2021). COVID-19 vaccines work well against California variant, scientists say. [online] Los Angeles Times. Available at: https://www.latimes.com/science/story/2021-04-07/covid-19-vaccines-work-well-against-california-variant.
- CDC (2020). Coronavirus Disease 2019 (COVID-19). [online] Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/ [Accessed 4 Jun. 2021].
- Corum, J. and Zimmer, C. (n.d.). Coronavirus Variants and Mutations. The New York Times. [online] Available at: https://www.nytimes.com/interactive/2021/health/coronavirus-variant-tracker.html#Q677.
- CDC (2020). Coronavirus Disease 2019 (COVID-19). [online] Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/.
- www.who.int. (n.d.). Tracking SARS-CoV-2 variants. [online] Available at: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/.
- Science Brief: Omicron (B.1.1.529) Variant [Online]. Available from: https://www.cdc.gov/.
- This map shows where the Covid omicron variant has been detected [Online]. Available from: https://www.cnbc.com/2021/12/02/interactive-map-shows-where-the-covid-omicron-variant-has-been-detected.html.
-
Variants. CDC. https://www.cdc.gov/coronavirus/2019-ncov/variants/index.html
-
Data Tracker. CDC. https://covid.cdc.gov/covid-data-tracker/#datatracker-home
SARS-CoV-2 variants of concern as of 15 December 2023. ECDC. https://www.ecdc.europa.eu/en/covid-19/variants-concern
-
Nyberg, T. et al. (2023). A standardised protocol for relative SARS-CoV-2 variant severity assessment, applied to Omicron BA.1 and Delta in six European countries, October 2021 to February 2022. Euroroundup, 28(36). https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2023.28.36.2300048?crawler=true
Further Reading
Last Updated: Jun 14, 2024