
Immunity. Image Credit: Yurchanka Siarhei/Shutterstock.com
The immune system – innate and adaptive
The immune system encompasses a collection of biological processes that are tasked with protecting the organism against infection and disease. It is capable of responding to a vast array of pathogens (ranging from cancer cells to viruses), targeting these agents and implementing measures through which the danger can be mitigated or wholly neutralized.
The immune system encompasses a collection of biological processes that are tasked with protecting the organism against infection and disease. It is capable of responding to a vast array of pathogens (ranging from cancer cells to viruses), targeting these agents and implementing measures through which the danger can be mitigated or wholly neutralized.
Broadly speaking, the manner in which the immune system counteracts pathogenic agents can be divided into two categories: the innate and adaptive immune responses.
The innate response refers to a generic, non-specific set of actions and processes the immune system puts into motion on the detection of a potential pathogen, typically through the activation of pattern recognition receptors (PRRs).
In general, this response is short-lived and does not result in the development of long-lasting immunity. This task is instead performed through the activation of the adaptive immune response, wherein specific pathogens can be recognized by the immune system potentially years after the point of first contact.
This ability is extremely useful as it results in the implementation of antigen-specific responses, thus increasing system efficiency and vastly reducing the time taken to deal with the pathogenic threat.
The microbiome
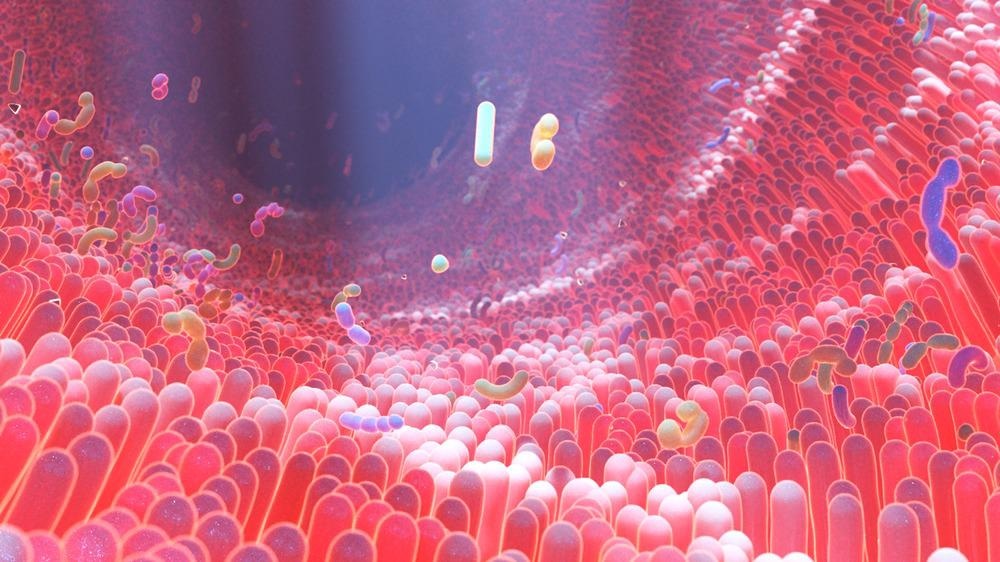
In a similar manner to how the immune system encompasses all immune-related agents and processes, the microbiome refers to the sum of all microbiota (e.g., bacteria, viruses, fungi, archaea) that are found within the human body.
Humans serve as the host for a wide plethora of microbes, with their total number being roughly equal to the number of human cells.
The relationships they have with their human host vary from species to species, with some microbes playing symbiotic or mutualistic roles while the function of others is still largely unknown.
Microbiome/immune system co-existence
The microbiota located in the intestinal tract have developed a mutually beneficial coexistence with the host during homeostasis and induce immune tolerance to commensal microbes, even as the immune system continues to respond to invading pathogens.
The detection of microbiota by PRRs induces several biochemical pathways which promote its commensal relationship with the immune system while also eliminating pathogenic infections. For example, pro-inflammatory cytokines such as IL-23 can be induced through the sensing of microbial components and/or metabolites, which in turn are capable of activating pathways that result in the generation of antimicrobial peptides (AMPs).
As well as this, some gut bacteria are involved in the fermentation of dietary fibers, resulting in the production of small chain fatty acids (SCFAs) which in turn promote the release of anti-inflammatory cytokines.
The microbiome. Image Credit: Alpha Tauri 3D Graphics/Shutterstock.com
Dysfunction of microbiome-immune system interaction in disease
It has been found that the irregular interactions between the microbiome and the immune system in genetically predisposed hosts could potentially contribute to the occurrence of immunity-related diseases. Two highly relevant examples of this can be found in the prevalence of both rheumatoid arthritis and cancer.
Rheumatoid Arthritis (RD): RD is an autoimmune disorder involving inflammation and gradual disintegration of cartilage in the joints. An increase in the prevalence of Prevotella Copri has been shown to be evident in new-onset RA patients. Another study reported a strong correlation between RA and Collinsella; a bacteria which is known to be associated with IL-17A, a pro-inflammatory cytokine.
Microbiome metabolites (such as SCFAs) have also been reported to interact with multiple different RA-associated pathways. However, the causal relationship between the microbiome and RA is still not fully understood.
Cancer: Recent studies have suggested that crosstalk between the gut microbiota and the immune system plays an important role in cancer detection and inhibition by the immune system.
For example, NK cell (which target and eliminate cancerous cells and tumors) functionality has been shown to be directly inhibited by Fusobacterium nucleatum, at least in part through the binding of its Fap2 protein to the TIGIT receptor. As well as this, F. nucleatum has been linked with decreases in CD3+ T cell density in human colorectal cancer patients.
Both of these examples suggest that the microbiome can act deleteriously in cancer prevention. However, Clostridium found in the liver has been observed increasing the antitumoral effects of hepatic CXCR6+ NKT cells on liver tumors. Taken together, these findings imply that the microbiome’s role in cancer development or treatment can be bidirectional.
Interestingly, the microbiome has also been suggested as a modulator of current anticancer immunotherapies. Various commensal microbiota species, such as Bifidobacterium longum and Collinsella aerofaciens, have been reported to display an increase in prevalence in conjunction with higher efficacy of PD-1 blockade therapy (due to an increased T cell-mediated response) in metastasized melanoma patients.
A similar response involving an increase in the efficacy of anti-PD-1 therapy has been observed concomitant with increased fecal Akkermansia muciniphila, possibly due to lymphocyte recruitment as well as IL-12 secretion.
Current challenges and future directions
Research such as the examples listed above has highlighted the potential role of microbiome and immune system interaction in disease development and prognosis. It should be noted that there remains practical challenges in such investigations.
For example, studies involving the use of laboratory mice are problematic as firstly, the microbiome composition of mice is vastly different than that found typically in humans; and secondly, wild mice harbor divergent microbiota than what is found in laboratory mice.
Interestingly, wild mice appear to exhibit a gut microbiome that more closely resembles that found in humans, suggesting that future research should consider transplanting such microbiota in their test mice. As well as this, it is clear that there is a high degree of inter-individual variability in microbiome composition and immune responses. While this of course poses a challenge for current researchers, it also opens the possibility of developing highly personalized microbiome-targeting treatment strategies in the future.
Without a doubt, the microbiome offers a fascinating, novel route through which immune-related therapies can be modulated and hopefully amplified in their efficacy. Its role in general health and well-being is only now being elucidated, with further research likely to uncover further microbiota characteristics that could play a pivotal role in future treatment strategies.
References
- Kogut, M. H., Lee, A., & Santin, E. (2020). Microbiome and pathogen interaction with the immune system. Poultry science, 99(4), 1906-1913. https://www.sciencedirect.com/science/article/pii/S0032579119579226?via%3Dihub
- Levy, M., Thaiss, C. A., & Elinav, E. (2016). Metabolites: messengers between the microbiota and the immune system. Genes & development, 30(14), 1589-1597. http://genesdev.cshlp.org/content/30/14/1589.short
- Zheng, D., Liwinski, T., & Elinav, E. (2020). Interaction between microbiota and immunity in health and disease. Cell research, 30(6), 492-506. https://www.nature.com/articles/s41422-020-0332-7
Further Reading
Last Updated: Feb 21, 2022