Angiotensin receptor blockers are antihypertensive medicines used to treat high blood pressure. They act as vasodilators, widening the blood vessels (vasodilation) and reducing blood pressure.
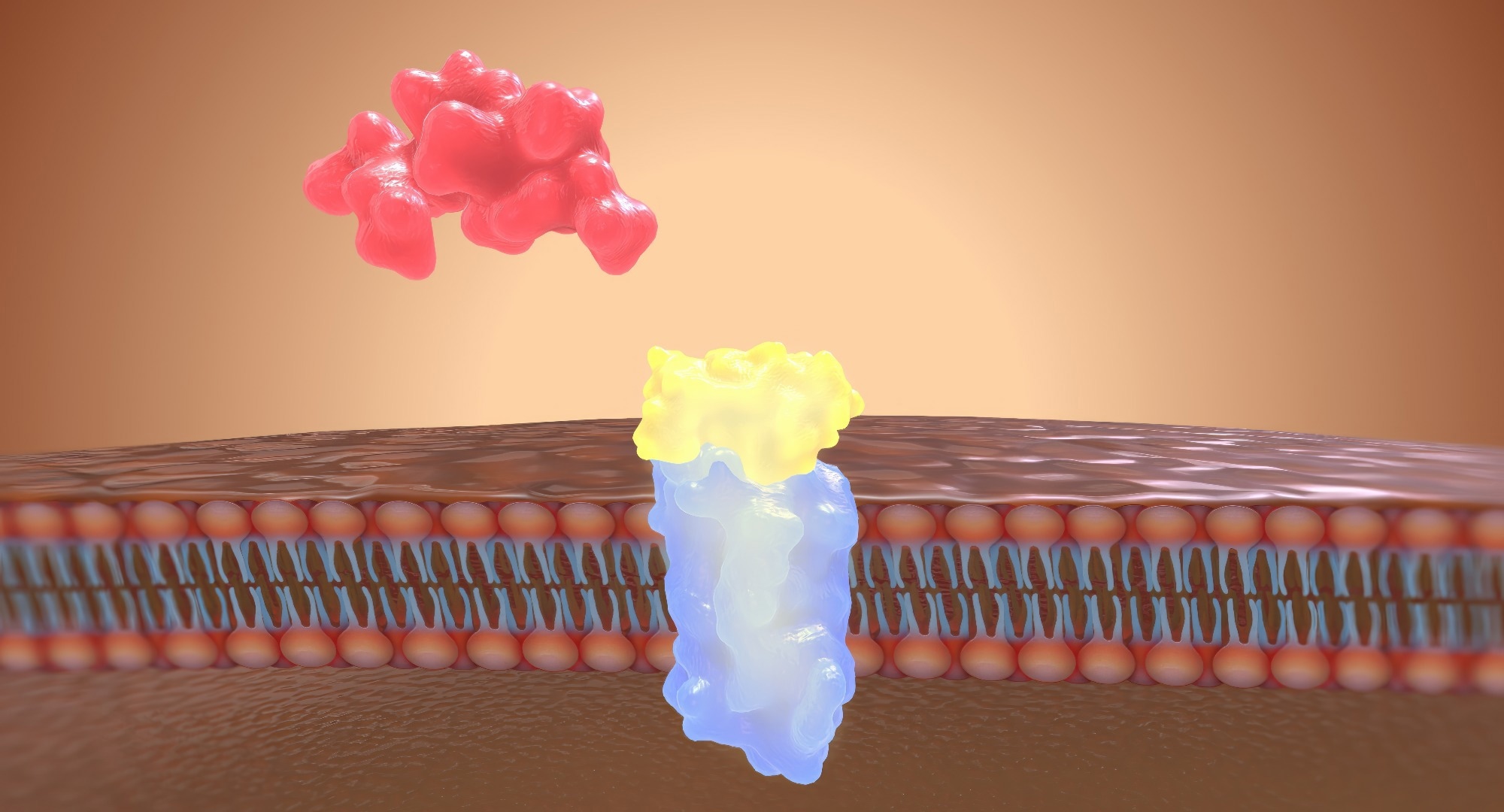 Image Credit: aipicte / Shutterstock
Image Credit: aipicte / Shutterstock
What is angiotensin?
The term ‘angiotensin’ collectively defines a group of four peptide hormones (angiotensin I—IV) that are crucial for blood pressure regulation. They are part of the renin-angiotensin-aldosterone system.
The first step of angiotensin synthesis is the hepatic formation of angiotensinogen (an inactive precursor), which is initially converted into angiotensin I by renin and then to angiotensin II by angiotensin-converting enzyme.
The renin-angiotensin-aldosterone system primarily comprises three vital biomolecules: renin, angiotensin II, and aldosterone. These biomolecules exert their effects on the kidney, lungs, vascular system, and brain.
The main function of the system is to regulate blood pressure and maintain fluid balance by increasing sodium and water retention and regulating vascular tone.
How angiotensin works?
Angiotensin, particularly angiotensin II, binds to angiotensin II receptors (type I and type II) and increases blood pressure in many ways.
In the kidney, angiotensin II increases sodium reabsorption, which in turn results in increased blood osmolarity and elevated arterial blood pressure.
In the adrenal cortex, angiotensin II induces the secretion of a steroid hormone, aldosterone, which acts by increasing the reabsorption of sodium and excretion of potassium. The net effect is increased blood volume and osmolarity, leading to increased blood pressure.
In the systemic arterioles, binding of angiotensin II to its receptor leads to vasoconstriction, which in turn causes induction of peripheral resistance and systemic blood pressure.
In the brain, angiotensin II acts on the hypothalamus to induce thirst sensation and increase water intake. Moreover, it acts on the posterior pituitary gland to induce the release of antidiuretic hormone, or vasopressin, which in turn causes retention of water in the kidney and elevation of the blood volume.
Lastly, angiotensin II prevents baroreceptor-mediated regulation of blood pressure by reducing receptor sensitivity.

Image Credit: Kateryna Kon/Shutterstock.com
What are angiotensin receptor blockers?
Angiotensin receptor blockers, or angiotensin II receptor antagonists, are used to treat high blood pressure, heart failure, chronic kidney diseases, and diabetic nephropathy. They inhibit the action of angiotensin II by blocking the ligand-receptor interaction.
In simple words, angiotensin receptor blockers dilate or widen the blood vessels so that blood can flow easily through the circulation. They also regulate blood volume by reducing sodium and water retention.
Angiotensin receptor blockers are particularly helpful when the body's angiotensin II level is too high. Too high angiotensin II levels can lead to excessive fluid retention, sustained increases in blood pressure, and heart expansion, which may ultimately cause heart failure.
However, too low angiotensin II can be detrimental as well. It can lead to abnormal blood volume regulation, increased potassium retention, and excessive loss of sodium and water, which altogether can cause significantly low blood pressure.
What are the side effects of angiotensin receptor blockers?
Angiotensin receptor blockers usually do not have side effects. Some people, however, can develop mild side effects due to the consumption of new medicine or due to having a higher dose of the medicine.
The most common side effects include dizziness, headache, fatigue, flu-like symptoms, a higher blood potassium level, or skin swelling due to fluid accumulation (angioedema).
In some rare cases, the blockers can cause severe diarrhea and loss of body weight. These symptoms call for immediate medical attention.
Women who are pregnant or planning to become pregnant should not take these blockers because of the possible harmful effects on fetal development.
Do angiotensin receptor blockers react with other medicines?
It is not recommended to take the blockers along with angiotensin-converting enzyme inhibitors. Taking both medicines together can lead to very high blood potassium levels, which can further increase the risk of acute kidney injury and heart rhythm abnormalities.
In addition, certain painkillers and mild potassium-sparing diuretics can increase the risk of high blood potassium levels if taken together with the blockers.
For better results, people consuming angiotensin receptor blockers should limit their salt intake. Also, too much alcohol consumption can increase blood pressure and reduce the efficacy of the blockers.
What are the benefits of angiotensin receptor blockers?
Angiotensin receptor blockers have several benefits. In addition to reducing the risk of cardiovascular and kidney disorders, these blockers prevent organ damage and comorbidities caused by high blood pressure. The comorbid conditions that get maximum benefits from angiotensin receptor blockers include diabetes, microalbuminuria, and left ventricular dysfunction.
Most importantly, the blockers inhibit the functions of angiotensin II by directly blocking the receptor. This is more advantageous than reducing the level of angiotensin II in the body.
Moreover, studies have shown that the adherence to angiotensin receptor blocker-mediated therapies is higher than that observed in other antihypertensive medicines. Good treatment adherence is associated with better management of blood pressure.
Angiotensin receptor blockers and epilepsy
Recent research has shown that angiotensin receptor blockers appear to reduce adults' risk of developing epilepsy. The finding comes from an analysis of the medical records of more than 2 million Americans taking blood pressure medications.
The study, published June 17, 2024, in JAMA Neurology, suggests that the drugs could prevent epilepsy in people at the highest risk of the disease, including older adults who have had strokes.
References
Further Reading
Last Updated: Jun 18, 2024