The renin-angiotensin-aldosterone system (RAAS), or renin-angiotensin-system (RAS) is a regulator of blood pressure and cardiovascular function. Dysregulated RAAS is implicated in high blood pressure, cardiovascular and kidney conditions, and medications targeting RAAS can improve these conditions.
Dysfunction of the RAAS is also thought to be implicated in COVID-19 severity and targeting RAAS may be a potential therapeutic strategy for COVID-19 complications.
 Image Credit: kurhan/Shutterstock.com
Image Credit: kurhan/Shutterstock.com
What is the renin-angiotensin-aldosterone system (RAAS)?
The RAAS is a complex multi-organ endocrine (hormone) system involved in the regulation of blood pressure by balancing fluid and electrolyte levels, as well as regulating vascular resistance & tone. RAAS regulates sodium and water absorption in the kidney thus directly having an impact on systemic blood pressure.
Typically, RAAS is activated when there is a drop in blood pressure (reduced blood volume) to increase water and electrolyte reabsorption in the kidney; which compensates for the drop in blood volume, thus increasing blood pressure.
Renin
Juxtaglomerular cells in the kidney are abundant in an inactive precursor protein called prorenin which is constantly secreted. Decreased blood pressure activates juxtaglomerular cells, which leads to prorenin being cleaved into its active form – renin, which is then secreted into the bloodstream.
Angiotensin
Renin acts on angiotensin (continuously produced by the liver) to cleave a 10 amino acid peptide from the N-terminus to form angiotensin I (inactive). Angiotensin-converting-enzyme (ACE) further cleaves angiotensin I to form angiotensin II – which is the primary active peptide of RAAS. ACE is primarily found in vascular endothelia of the lungs and the kidneys.
Angiotensin II binds to angiotensin type I A (AT1AR) or B (AT1BR), as well as type II (AT2R) receptors. Angiotensin II is a potent vasoconstrictor, which leads to increased blood pressure. Normally, if blood pressure is too high, atrial natriuretic peptide (ANP) – secreted by cardiac muscle cells – leads to reductions in blood volume, leading to reduced blood pressure.
Angiotensin II binding to AT1R can result in a cascade of inflammation, constriction, and the promotion of atherosclerosis. Furthermore, these events can also lead to insulin resistance and thrombosis, whereas binding to AT2R has opposing effects: vasodilation reduced platelet aggregation and enhanced insulin activity.
Angiotensin II also acts on the brain where it can bind to the hypothalamus to stimulate thirst to increase water intake. By acting on the pituitary gland, angiotensin II also stimulates the secretion of vasopressin; also known as antidiuretic hormone, which increases water retention in the kidneys by adding water channels (aquaporin) to the collecting duct.
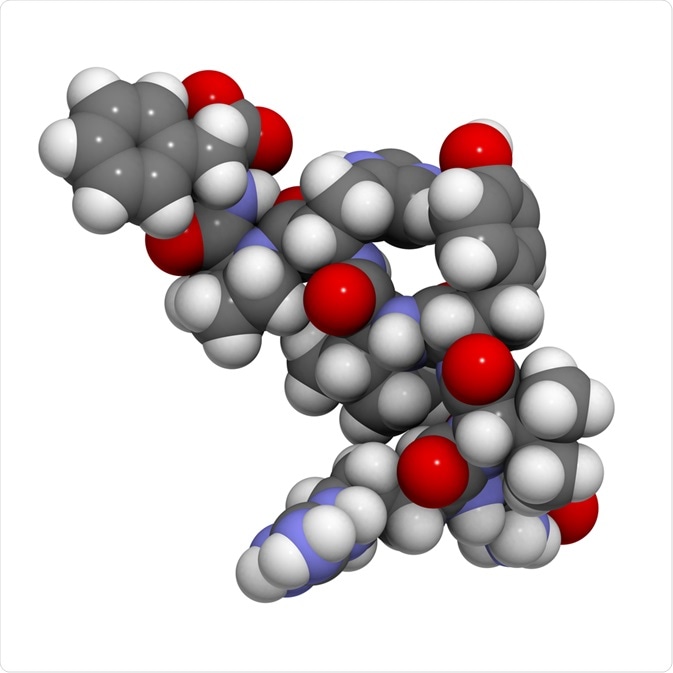 Angiotensin II structure. Image Credit: StudioMolekuul/Shutterstock.com
Angiotensin II structure. Image Credit: StudioMolekuul/Shutterstock.com
Aldosterone
Angiotensin II stimulates the secretion of aldosterone is produced by the zona glomerulosa of the adrenal cortex (adrenal gland) and is involved in the retention of sodium in the kidney and other glands. The retention of water and sodium leads to increased blood volume, and thus blood pressure.
Dysfunctional RAAS
Primary pathologies of impaired RAAS include chronic hypertension, kidney, and cardiac failure. Abnormally active RAAS leads to chronic hypertension and thus the high blood pressure needs to be counterbalanced.
ACE inhibitors are commonly used drugs in the treatment and management of hypertension and heart failure. ACE inhibition prevents the conversion of angiotensin I to angiotensin II, thus keeping angiotensin inactive.
Angiotensin II binding to AT1R can also induce cardiac dysfunction including hypertrophy, arrhythmia, and ventricle function failure. Excessive angiotensin II can also lead to large inflammatory changes such as cytokine-induced organ damage in addition to increased membrane permeability and epithelial cell apoptosis.
As angiotensin II is a vasoconstrictor, alleviation causes vasodilation thus reducing systemic blood pressure levels. ACE inhibitors also lead to the increased production of bradykinin – which is a vasodilator. Other drugs include angiotensin receptor blockers (ARBs) – which block the binding of angiotensin II to ATRs. ACE inhibitors and ARBs are also effective drugs in the management of heart failure and complications of diabetes.
In the kidney, renal arterial stenosis leads to decreased blood volume entering the kidneys; consequently, juxtaglomerular cells sense a decreased blood volume and RAAS is activated. This, negatively, enhances blood pressure further which is inappropriate to the systemic circulation as well as increasing arterial tone. Thus, ACE inhibitors and ARBs can also be used in patients with renal arterial stenosis to limit the inappropriate activation of RAAS.
RAAS and COVID-19
The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), uses ACE2 to gain entry into respiratory epithelial cells (along with TMPRSS2). When SARS-CoV-2 binds to ACE2, the activity of ACE2 is downregulated, preventing its normal function and leading to respiratory symptoms of cough and edema, as well as upregulation of angiotensin II.
.jpg) SARS-CoV-2 binds to ACE2 receptor on human cells. Image Credit: Kateryna Kon/Shutterstock.com
SARS-CoV-2 binds to ACE2 receptor on human cells. Image Credit: Kateryna Kon/Shutterstock.com
Furthermore, a link between RAAS dysfunction in hypertension and cardiovascular disease and enhanced COVID-19 complications and fatality has also been suggested (RAAS-SCoV-axis).
COVID-19 complications and mortality rates are higher in patients with hypertension and cardiac/cardiovascular diseases and may reflect aberrant RAAS (increased angiotensin II and reduced ACE2).
As previously mentioned, angiotensin II binding to AT1R can lead to inflammation leading to tissue injury originating from lung epithelial cells. This may lead to acute respiratory distress syndrome (ARDS). Angiotensin II binding to AT2R can reverse the negative effects of AT1R binding (discussed above).
However, it is important to note that the expression of AT2R is relatively low in normal healthy adults, thus the primary modulatory effects upon angiotensin II are mediated by ACE2, converting angiotensin II into lung-protective angiotensin-(1-7/1-9) (opposing ACE).
Elevated ACE2 expression may be compensatory in patients with cardiovascular disease and heart failure. Indeed, influenza and coronaviruses (along with viral forms of pneumonia), tend to see reduced ACE2 expression and upregulation of angiotensin II.
Thus, there is a theory that those with overactive RAAS (enhanced angiotensin II and ACE2 expression) may be at a higher risk of developing severe pathology as a result of SARS-CoV-2 infection.
In healthy adults, the expression of ACE2 is low, and ACE2 expression may be an independent predictor for COVID-19 risk and severity as the SARS-CoV-2 virus utilizes ACE2.
Furthermore, women have a higher expression of AT2R compared to men (as ACE2 is on the X-chromosome), and this may reflect that COVID-19 infections and complications tend to be higher in men.
ACE inhibitors and ARBs lead to increased renin and angiotensin I levels (inactive) and inhibit angiotensin I to II conversion, thus protecting the body from the negative effects of angiotensin II to AT1R binding (as discussed).
ARBs, however, lead to increased angiotensin II levels. This is then directed towards ACE2 modulation and AT2R binding to have protective effects. Thus, ARBs may be better than ACE inhibitors at rebalancing the RAAS pathway. ARBs have been posited as a therapeutic avenue for COVID-19.
Treating COPD patients with ARBs can lead to lower mortality and reduced need for mechanical ventilation. Furthermore, those on ARBs before hospitalization for pneumonia have a decreased mortality rate compared to those not using ARBs.
There are many associations between angiotensin II levels and prediction of mortality for influenza, and those using RAAS inhibitors (ARBs) often do not need intubation in those with viral pneumonia. This seems to be the same for COVID-19, and RAAS drugs may be protective in reducing the complications and need for hospitalization.
Whilst the possibility of using ARBs or ACEIs as a therapy for COIVD-19 still needs to be looked into and further researched, studies such as that of Wang et al. (2021) suggest that the use of ACEIs and ARBs is safe to treat COVID-19 induced pneumonia.
Recent studies like the randomized clinical trial carried out by Lopes et al. (2021) have come to the conclusion that those already taking ACEIs or ARBs before hospital admission should not discontinue if hospitalized with mild to moderate COVID-19.
To summarise the link between COVID-19 and RAAS, SARS-CoV-2 binds to ACE2 to gain entry into respiratory epithelial cells. Normally angiotensin II binding to AT1R causes negative effects and these effects can be modulated by ACE2 and AT2R binding.
However, SARS-CoV-2 reduces ACE2 expression, thus leading to lung injury by a cascade of inflammation. ACE inhibitors and ARBs may rebalance the RAAS pathway to favor ACE2 function to oppose the negative effects of angiotensin II and converting it to a lung-protective angiotensin-(1-7).
Many patients with viral pneumonia and COPD taking ARBs tend to have better prognoses than those without – especially with respect to hospitalization and mortality. Needless to say, the association between SARS-CoV-2 and ACE2 interaction as part of RAAS (RAAS-SCoV-axis) is still poorly understood and needs much further investigation at this stage.
The Renin–Angiotensin–Aldosterone System, RAAS, Animation
Summary
In summary, the renin-angiotensin-aldosterone system (RAAS) is a critical regulator of blood pressure (blood volume & electrolyte balance) as well as vascular tone & resistance. Normally, renin is secreted if blood pressure is too low thus activating angiotensin II to increase blood pressure and vascular resistance.
Abnormal activation of RAAS leads to chronic hypertension, cardiac failure, and kidney conditions, and may be a predictor for risk of complication in COVID-19. Drugs inhibiting the RAAS pathway such as ACE inhibitors and ARBs are effective treatments for hypertension and cardiac failure and maybe an important option for minimizing COVID-19 complications.
References
[further reading: coronavirus disease COVID-19]
Last Updated: Mar 4, 2021