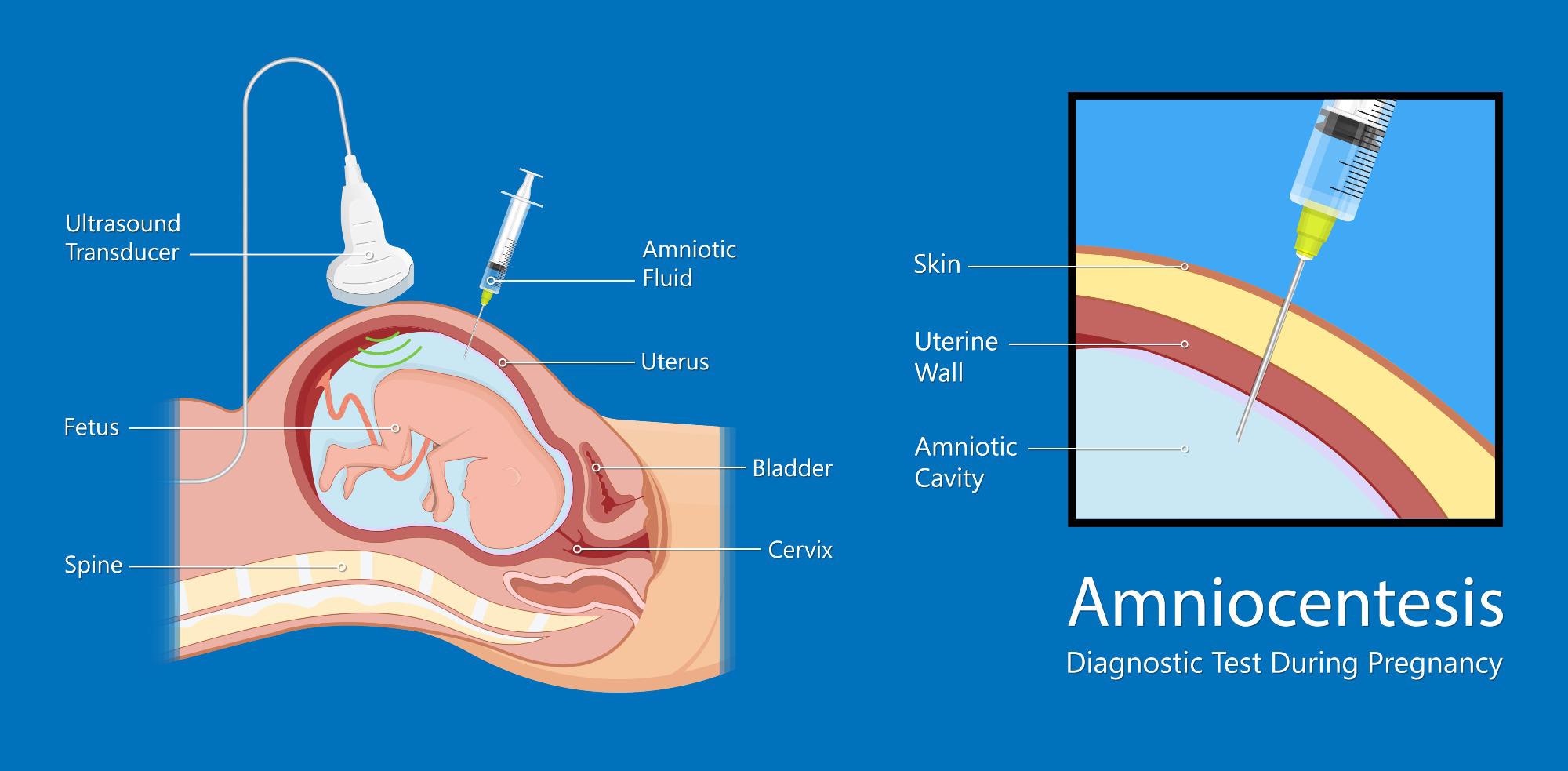
Amniocentesis describes the extraction of amniotic fluid through the abdominal wall (i.e., through a transabdominal approach with ultrasound guidance). This procedure is performed by a trained obstetrician or gynecologist. The amniotic fluid extracted contains fetal cells alongside transudates such as epithelial and bladder cells.

Amniocentesis. Image Credit: Thomas Andreas/Shutterstock.com
Why is amniocentesis performed?
Amniocentesis is employed to detect chromosome abnormalities and has two indications:
- Diagnostic: in this case, it is used for chromosomal analysis. Specifically, karyotyping and DNA analysis are performed to diagnose sex-linked disorders, neural tube defects, and inborn errors of metabolism. It is performed in the case of:
- Advanced maternal age i.e, >35 years
- The presence of abnormal biochemical screening markers in the mother, such as maternal alpha-fetoprotein, human chorionic gonadotrophin, and unconjugated estriol seen in the first or second trimester
- The ultrasound detection of an abnormality or soft tissue marker
- Family or personal history of the chromosome will abnormalities
- Evaluation of fetal lung maturity, fetal anemia, and infection, platelet and blood type determination
- Diagnosis of chorioamnionitis
- Therapeutic: In the context of therapeutic application, it is performed to reduce the quantity of amniotic fluid in women suffering from polyhydramnios. Polyhydramnios is the excessive accumulation of amniotic fluid; it is associated with an increased risk of perinatal morbidity and mortality. In oligohydramnios ( too little amniotic fluid) it is used to prevent fetal lung hypoplasia and umbilical cord compression during labor.
Early measures, however, can lead to increased unsuccessful cell cultures, a higher risk of miscarriage, and fetal complications. The most salient issue in amniocentesis is the occurrence of early abortion. The statistics reporting on the incidence rate of miscarriage are wide, but the highest reported numbers go up to 10%.
When is amniocentesis performed?
Amniocentesis is typically performed between 15 and 17 weeks of gestation. Within this time frame, the window can be shifted, to allow amniocentesis to be performed earlier, between 11 and 14 weeks of gestation. The risk of miscarriage is the most salient risk due to the absence of fused membranes; alongside the risk of miscarriage, there is an increased risk of procedure-related complications. This includes increased risk of amniotic fluid leakage, intrauterine fetal demise (IUFD), or stillbirth, and clubfoot, also known as talipes equinovarus. Before the procedure is performed, the couple is counseled regarding indications, risks, benefits, and limitations.
Amniocentesis. Image Credit: rumruay/Shutterstock.com
The physiology of amniotic fluid
Amniotic fluid functions as a non-sterile aqueous electrolyte solution. In the early weeks of gestation, the fetus's skin is not keratinized, which allows for the free transfer of water and other small molecules and solutes through the amnion and the chorion.
The amnion is located in the innermost part of the placenta where it lines the amniotic cavity. Its purpose is to contain the amniotic fluid and the developing embryo. The chorion, however, is the extraembryonic, outer membrane, that surrounds the amnion, the embryo, and other membranes and entities in the womb.
During the second trimester of pregnancy, diffusion stops, and characterization of the fetal skin occurs. This makes the fetal skin impermeable to water and solutes. The composition of the amniotic fluid changes throughout gestation. At 9 weeks, urine is observed in the fetal bladder and on transabdominal sonography and urine is visible at 11 weeks of gestation. At this point, the predominant constituent of amniotic fluid is fetal urine; This urine is hypotonic (contains a lower concentration of solutes relative to the fetus). The fetal kidneys contain an increasing concentration of urea, uric acid, and creatinine as they mature. At full term, a fetus can produce between 500 and 700 ml of urine in a day.
Maternal complications of amniocentesis
Both maternal and fetal complications can arise as a result of amniocentesis. In the case of maternal complications, fetal-maternal hemorrhage carries an approximate 2.6% risk. Other risks include:
- Maternal isoimmunization in Rh-negative cases: Rh factor is a protein on red blood cells. Rh isoimmunization is when the fetal blood stimulates the production of maternal antibodies against the fetal blood.
- Increased risk of preterm, premature rupture of membrane, and oligohydramnios
- 2% to 3% risk of vaginal bleeding
- Post-procedure pain and maternal discomfort
- Amniotic fluid embolism: amniotic fluid, fetal cells, hair, or other debris enters the maternal pulmonary circulation, causing cardiovascular complication
- Hematoma: localized bleeding outside of blood vessels, typically on skin, intestinal or internal organ injures.
References
- Tara F, Lotfalizadeh M, Moeindarbari S. (2016) The effect of diagnostic amniocentesis and its complications on early spontaneous abortion. Electron Physician. doi:10.19082/2787
- Jindal A, Sharma M, Chaudhary C. Amniocentesis. [Updated 2021 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559247/
- Jummaat F, Ahmad S, Mohamed Ismail, NA. (2019) 5-Year review on amniocentesis and its maternal fetal complications. Horm Mol Biol Clin Investig. doi: 10.1515/hmbci-2019-0006.
Further Reading
Last Updated: May 4, 2022