Introduction
What are neutrophils?
Homeostatic regulation of neutrophils
What is neutropenia?
Primary causes of neutropenia
Secondary neutropenia
Diagnosis
Management and treatment
References
Further reading
Introduction
Neutrophilic granulocytes, which are otherwise known as neutrophils or polymorphonuclear (PMN) leukocytes, are the most abundant circulating white blood cells in humans. Thus, neutrophils play a fundamental role in the innate immune response.
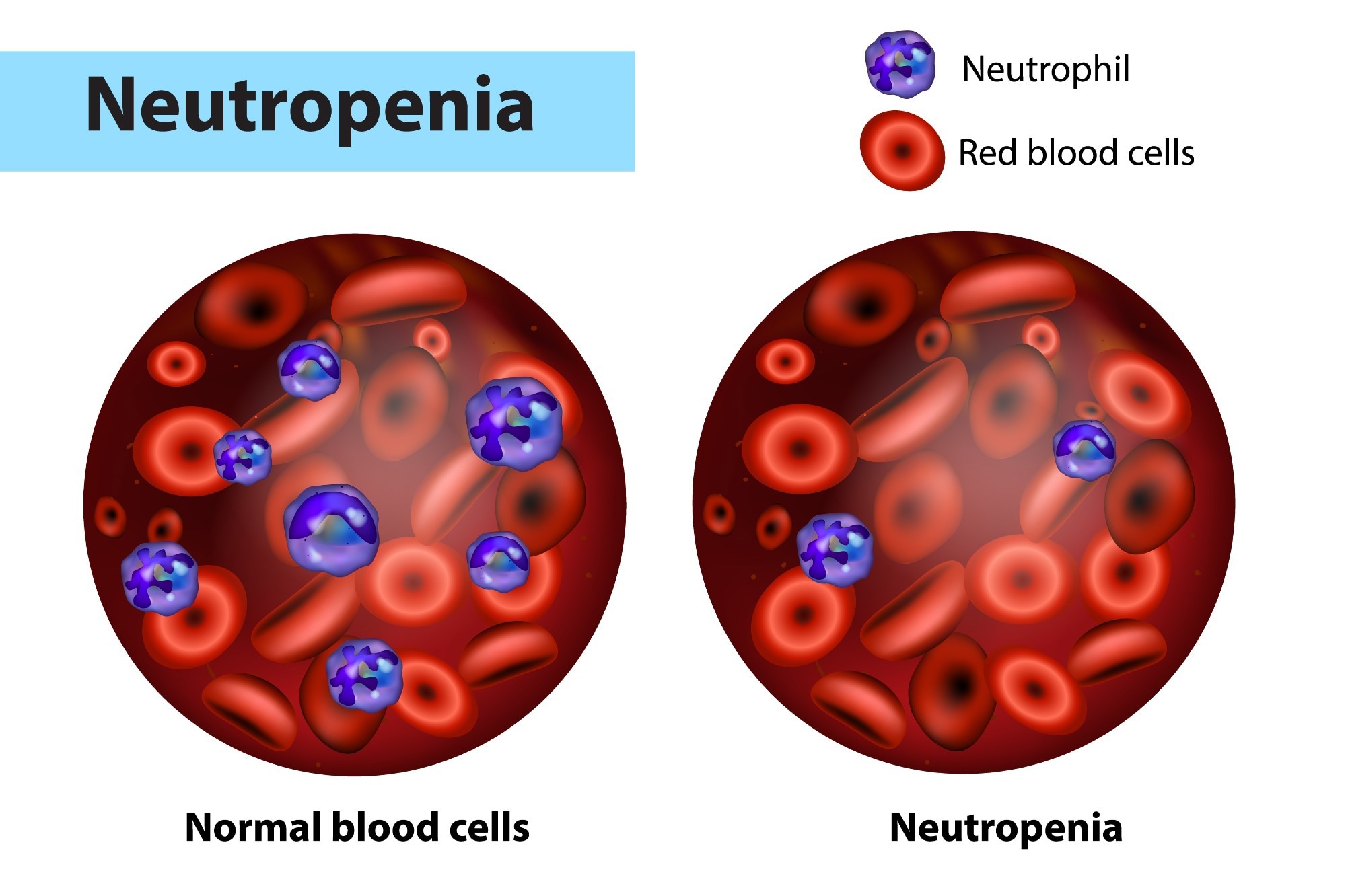 Neutropenia and normal blood cells. Image Credit: Sakurra / Shutterstock
Neutropenia and normal blood cells. Image Credit: Sakurra / Shutterstock
What are neutrophils?
The primary function of neutrophils, the first cells to respond to invading pathogens, is to kill invading microorganisms through phagocytosis. Phagocytosis involves the digestion of the pathogen by the neutrophil into a phagocytic vacuole, which subsequently leads to the destruction of the microorganism by the low pH of this new organelle and granular enzymes.
Thereafter, neutrophils will undergo degranulation, which leads to the release of cytokines and other inflammatory factors. In addition, neutrophils can also produce neutrophil extracellular traps (NETs), which consist of the DNA fibers and proteins from the released granules. These actions by neutrophils can also lead to the production of reactive oxygen species (ROS), which has a vital role in the inflammatory response to pathogens.
Neutrophils within the blood, originating from precursor cells within the bone marrow, can be categorized as peripheral or circulating neutrophils. Whereas peripheral neutrophils are attached to the vascular endothelial, circulating neutrophils freely circulate throughout the bloodstream.
Homeostatic regulation of neutrophils
Stable neutrophil blood counts are not static but rather a result of a highly dynamic feedback system. Neutrophil homeostasis is maintained by a delicate balance between granulopoiesis, which describes the production of granulocytes, bone marrow storage and release, margination in blood vessels, clearance, and destruction.
Neutrophils are produced inside the hematopoietic cords interspersed within the venous sinuses of the bone marrow. The differentiation of granulocytes is regulated by the synchronized expression of fundamental myeloid transcription factors, with granulocytes and macrophages differentiating from a common progenitor cell.
Neutrophil counts in healthy humans are regulated by a myriad of environmental and genetic factors, most of which remain unknown. The presence of severe neutropenia highlights the vital role of the neutrophil, with its panoply of defense mechanisms used to contain and kill pathogenic microorganisms.
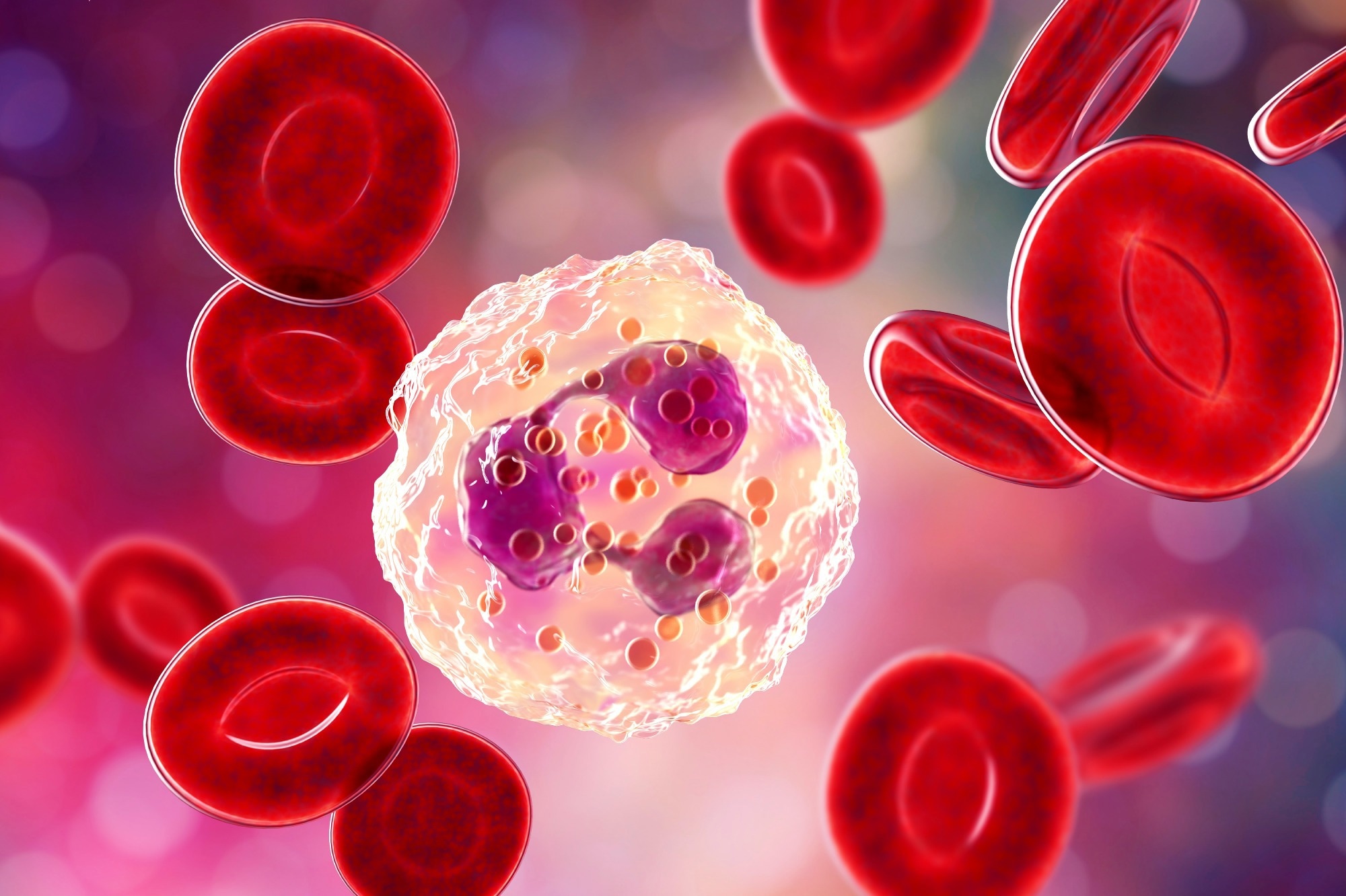 Neutrophil, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
Neutrophil, 3D illustration. Image Credit: Kateryna Kon / Shutterstock
What is neutropenia?
In healthy individuals, the neutrophil count within the blood, which is referred to as the absolute neutrophil count (ANC), is typically within the range of 2,500 and 7,000 neutrophils per microliter (µl) of blood.
Neutropenia can be defined as the reduction in the absolute number of neutrophils in blood circulation. This blood condition can be classified as acute or chronic, as well as primary or secondary.
Acute neutropenia arises when neutrophil use is rapid and production impaired; conversely, chronic neutropenia results from reduced production, increased destruction, or excessive splenic sequestration of neutrophils, often lasting three months or more.
Primary causes of neutropenia
In primary neutropenia, reduced neutrophil levels limit the ability of the innate immune system to respond to pathogens, thus increasing the risk of recurrent infections in these patients. Notably, primary neutropenia is considered a milder form of this blood condition than when it arises due to secondary causes, particularly as a result of chemotherapy treatment.
Primary acute neutropenia typically occurs in children who have been diagnosed with congenital disorders like chronic granulomatous disease (CGD), leukocyte adhesion deficiency (LAD), reticular dysgenesis, Shwachman-Diamond-Oski syndrome, Chediak-Higashi syndrome, dyskeratosis congenita, hyper immunoglobulin M (IgM) syndrome, common variable immunodeficiency, severe combiner immunodeficiency, benign ethnic neutropenia (BEN), Kostmann syndrome, and cyclic neutropenia.
BEN is a chronic congenital form of neutropenia that typically causes ANC to be less than 1,500 neutrophils/μL. BEN is the most common cause of neutropenia among people from Africa, the Middle East, and West India.
LAD is an autosomal recessive condition that prevents peripheral neutrophils from adhering to endothelial cells, thus rendering them unable to ingest and kill bacteria. Chediak-Higashi syndrome is another type of autosomal recessive disorder in which neutrophils are unable to reach invading pathogens due to the lack of the lysosomal trafficking regulator protein.
Kostmann syndrome, which is otherwise known as severe congenital neutropenia autosomal recessive 3, causes affected individuals to have ABC of less than 500 cells/mm3. Importantly, the bone marrow of patients with Kostmann syndrome cannot produce mature neutrophils.
Cyclical neutropenia is characterized by a cyclic pattern of varying neutrophil counts, with a typical cycle duration of 21 days and periods of neutropenia lasting between three and five days. This condition arises due to fluctuating neutrophil production rates of the bone marrow stem cells. While cyclic neutropenia can occur sporadically, it is often due to a genetic mutation.
Another form of neutropenia is chronic idiopathic neutropenia. This is a relatively rare condition that can occur at any age for unknown reasons.
Secondary neutropenia
Secondary causes of neutropenia are more common than primary forms of neutropenia. Secondary neutropenia often arises due to autoimmune disorders such as rheumatoid arthritis, inflammatory bowel disease (IBD), chronic autoimmune hepatitis, granulomatosis with polyangiitis, Hodgkin lymphoma, and Sjorgen syndrome. Chemotherapy and radiation treatment may also lead to neutropenia.
Febrile neutropenia is the most common and severe complication associated with cancer treatments. This condition is characterized by an oral fever higher than 38.3°C with ANC less than 1,000 neutrophils/μL. Febrile neutropenia continues to represent a significant cause of morbidity, mortality, and economic loss in cancer and transplant patients receiving chemotherapy.
Some of the different drugs that are known to cause neutropenia include:
- Quinidine
- Aminopyrine
- Cephalosporin
- Sulfonamides
- Hydralazine
- Penicillins
- Heavy metals
- Phenothiazine
- Rituximab
- Procainamide
Other factors that increase the risk of neutropenia include viral, bacterial, and parasitic infections, such as human immunodeficiency virus (HIV), hepatitis, tuberculosis, sepsis, and Lyme disease. Furthermore, patients with health conditions that are associated with recurrent bacterial and fungal infections, such as diseases of the gastrointestinal (GI) and respiratory systems, are also at risk of neutropenia.
Nutritional deficiency of vitamin B12, folate, or copper can also cause neutropenia.
Diagnosis
There are no specific symptoms of neutropenia; however, the reduced levels of neutrophils associated with this condition often lead to bacterial and fungal infections such as tonsillitis, pharyngitis, mouth ulcers, and skin abscesses. In addition, severe fatigue, nausea, and loss of appetite may also be early signs of neutropenia.
A complete blood count (CBC) with differential is a simple test that can be used to determine if someone has neutropenia. This test is regularly performed to monitor neutrophil levels of cancer patients receiving chemotherapy, as nearly 50% of people receiving chemotherapy develop neutropenia.
Management and treatment
Care for patients with neutropenia is primarily supportive, with the cause, severity, and duration of the neutropenia carefully considered prior to determining the treatment protocol. Individuals with chronic or severe neutropenia must take additional precautions to protect themselves from contracting infections from food, other people, or the environment.
Fever and other types of infections that occur as complications of neutropenia necessitate specific and targeted treatment. Therefore, a surgical approach is usually not indicated but may be employed in specific contexts.
To combat infections, intravenous antibiotic treatment is often indicated in treating patients with febrile neutropenia. Likewise, patients with autoimmune neutropenia are often prescribed corticosteroids to suppress their body’s immune system.
The United States Food and Drug Administration (FDA) has approved granulocyte colony-stimulating factor (G-CSF) to reduce infection incidence among patients at risk of neutropenia. More specifically, the patients who may be prescribed G-CSF include those with specific malignancies who are currently receiving cancer treatments that increase their risk of febrile neutropenia. Additionally, patients who have previously received a stem cell transplant and are currently receiving chemotherapy and those with congenital forms of neutropenia.
Neutropenia - Mayo Clinic
References
- Rosales, C. (2018). Neutrophil: A Cell with Many Roles in Inflammation or Several Cell Types? Frontiers in Physiology 9(113). doi:10.3389/fphys.2018.00113.
- Vaillant, A. A. J., & Zito, P. M. (2022). Neutropenia. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507702/.
- Neutrophils [Online]. Available from: https://my.clevelandclinic.org/health/body/22313-neutrophils.
- Neutropenia [Online]. Available from: https://my.clevelandclinic.org/health/diseases/21058-neutropenia
- What is Neutropenia? [Online]. Available from: https://neutropenianet.org/what-is-neutropenia/
- Types of Neutropenia [Online]. Available from: https://neutropenianet.org/what-is-neutropenia/types-of-neutropenia/
- Infection risk and neutropenia [Online]. Available from: https://bloodcancer.org.uk/understanding-blood-cancer/blood-cancer-side-effects/neutropenia/neutropenia/
- Mehta, H. M., Malandra, M., & Corey, S. J. (2016). G-CSF and GM-CSF in Neutropenia. Journal of Immunology 195(4); 1341-1349. doi:10.4049/jimmunol.1500861.
- Cyclic neutropenia [Online]. Available from: https://my.clevelandclinic.org/health/diseases/21081-cyclic-neutropenia.
- Punnapuzha, S., Edemobi, P. K., & Elmoheen, A. (2022). Febrile Neutropenia. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541102/.
Further Reading
Last Updated: Sep 14, 2022