There are numerous bacteria, archaea, and eukaryotes living in the human gut. Collectively, this is referred to as the “gut microbiota”. The gut microbiota offers benefits to the human host, such as strengthening the integrity of the gut, shaping the gut epithelium, providing protection against pathogens, synthesizing vitamins, and regulating the immune system.
A study by Gilliland and co. looked to see if certain bacteria are able to assimilate lipids from the environment. Using a Lactobacillus acidophilus culture, they found that cholesterol levels in the culture medium were reduced if the culture medium included bile and was placed in anaerobic conditions, which somewhat mimics the conditions within the human gut.
A further animal study showed that the levels of fats in the blood were not raised on a high-fat diet if L. acidophilus was also present. This was not replicated in human studies, although that could be due to the fact that a human population is more diverse compared to animals used in research.
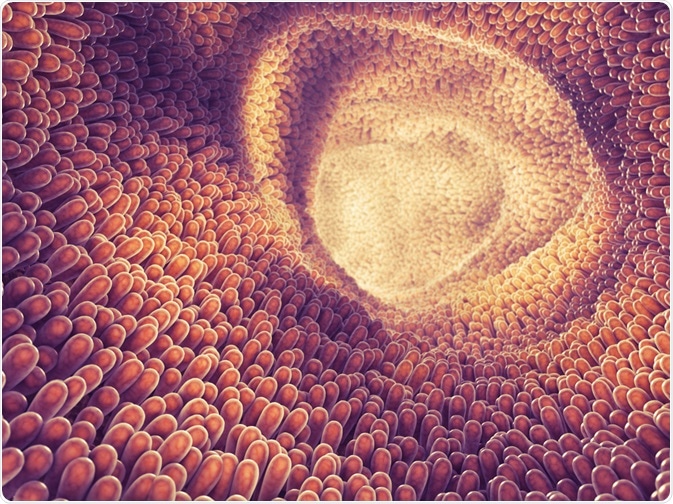 nobeastsofierce | Shutterstock
nobeastsofierce | Shutterstock
Lipids and the gut microbiota
Since the gut microbiota is clearly linked to the human host, does this mean that host metabolism is affected by the gut microbiota?
Studies have shown that the gut microbiota can affect the amount of energy that is extracted from food during digestion, which in turn can predispose individuals to obesity and the development of obesity-related illnesses such as insulin resistance and cardiovascular disease. Therefore, it is plausible that it can also have other effects on host metabolism.
Early studies that compared germ-free mice and conventionally raised mice suggested that the gut microbiota may play a role in host lipid metabolism. Given that there is a link between lipid levels and obesity, it is possible that the effect of certain bacterial taxa on host lipid metabolism is the same species that affect the host’s weight.
More recent studies have shown that taxa such as Akkermansia, Christensenellaceae, and Tenericutes were associated with obesity as well as triglycerides and high-density lipoprotein (HDL). Proportions of other taxa were shown to affect only lipid levels, such as Eggerthella, Pasteurellaeceae, and Butyricimonas.
A study looked at the association of blood lipid levels and the microbiota of 145 European women. This was a DNA sequencing-based approach, and abundant genes were categorized into “metagenomic gene clusters”. Each metagenomic gene cluster comprised of at least 104 genes, and 66 metagenomic gene clusters were shown to be associated with levels of triglycerides in the blood.
A further two metagenomic gene clusters were shown to be associated with blood HDL levels, however, there were no metagenomic gene clusters that were associated with low-density lipoprotein (LDL) or total cholesterol. One common metagenomic gene cluster between those which were associated with blood triglycerides and blood HDL came from the Clostridiales order.
Two studies showed that the functional richness of the gut microbiota was important in regulating levels of triglycerides and LDL cholesterol; functional richness was defined as “the total number of unique bacterial genes presented in an ecological community”.
Some 341 individuals were included in these two studies, and they showed that a reduced functional richness in the gut microbiota led to an increase in blood triglycerides and LDL cholesterol, as well as an increase in inflammation markers and increased insulin resistance.
Another study showed that 34 bacterial taxa were associated with BMI and blood lipids. Furthermore, volunteers who showed “unfavorable” blood lipids were found to have certain common themes in their gut microbiota; this included reduced diversity, higher levels of certain Actinobacteria taxa, and lower levels of certain taxa from Proteobacteria and Bacteroidetes, including Christensenellaceae, Pasteurellaeceae, and Butyricimonas.
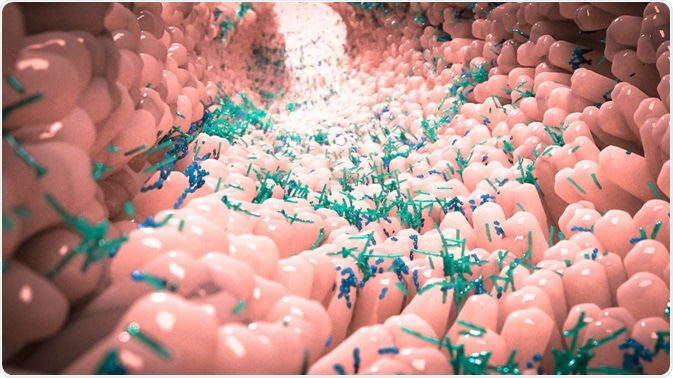 Alpha Tauri 3D Graphics | Shutterstock
Alpha Tauri 3D Graphics | Shutterstock
The Gut Microbiota, Host Lipid Metabolism, and Cardiovascular Disease
Coronary heart disease is a major cause of death in Western society. Risk factors of coronary heart disease include levels of triacyl glycerol and LDL/HDL cholesterol. Notably, diet is another major risk factor in the development of coronary heart disease, and modification of diet can change a person’s risk of coronary heart disease.
Studies have shown that there is a link between the Glycemic Index (GI) of a food and its effect on HDL-cholesterol in the blood. A low GI diet includes carbohydrates that are not easily digested, meaning that more would reach the gut microbiota. Other carbohydrates, such as fiber, cannot be digested by the host. The gut microbiota, on the other hand, has the capability to metabolize fiber and resistant starch, as well as the remaining carbohydrates from low GI foods.
Several studies showed that supplementation with fiber (inulin and oligofructose) lead to a reduction in the levels of lipids in the blood, with one by Brighenti and co. showing a significant decrease in blood triacylglycerol and cholesterol levels. However, other studies have shown no effect of dietary fiber supplementation on blood lipid levels. This effect could potentially be due to these fibers being fermented by the gut microbiota.
Further Reading
Last Updated: Sep 25, 2019