Jul 9 2012
A team of researchers at Trinity College Dublin’s School of Medicine has gained new insights into a protein in the human immune system that plays a key role in the protective response to infection and inflammation. The research findings have just been published in the internationally renowned peer-reviewed Journal of Biological Chemistry.
The TCD researchers investigated whether signalling via a protein known as the ‘LFA-1 integrin’ influences gene expression in immune cells called ‘T-cells’. In doing so, they discovered what is called “ a genetic signature”, that is a group of genes responding to the signal that make T-cells fail to respond to a controlling molecule called transforming growth factor-β (TGF-β).
“This is a bit like removing the handbrake and setting the immune system into action,” says Professor of Medicine, Dermot Kelleher who led the research.
The research may also have implications for treating inflammatory diseases where drugs targeting LFA-1 have had unacceptable and serious side effects such as progressive multi-focal leukoencephalopathy (PML) in the brain. “If we more fully understand the signalling mechanism leading to downstream gene regulation by LFA-1, we may be able to devise selective therapies to better treat various autoimmune diseases without major side effects such as PML,” according to Professor Kelleher.
Scientists have known for decades that LFA-1 is responsible for the majority of T-cell migratory behaviours associated with the immune response. Central to the success of immune responses that restrain inflammation are regulatory molecules, including a multifunctional cytokine TGF-β, which is essential for the development and function of an immune cell type, called the regulatory T-cells.
In the current study, Trinity College Dublin scientists conducted a genome wide analysis and detected that the expression of several genes were altered when T-cells were triggered to migrate to a site of inflammation through the interaction of LFA-1 with another protein called ICAM-1. This research was performed in collaboration with the Immunology Research Group at the National Children’s Research Centre at Our Lady’s Children’s Hospital, Crumlin led by SFI Stokes Professor of Translational Immunology, Padraic Fallon.
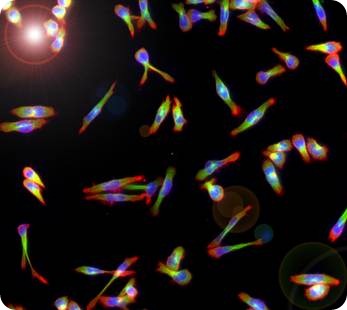
LFA-1 stimulated human peripheral blood lymphocyte T-cells fluorescently stained for tubulin (green), actin (red) and nuclei (blue).
“There is still much to learn about the genetic changes induced by the LFA-1 signal, but our studies are the first to show that a regulatory T-cells associated signal is influenced,” says TCD research fellow in clinical medicine, Dr Navin Kumar Verma, a lead author on the study. “The findings are novel and significantly contribute to the understanding of how the organism mounts an immune response. Several other genes identified here offer a general framework for future research in order to identify excellent targets for novel therapies for immune-mediated human diseases such as rheumatoid arthritis or inflammatory bowel disease.”
The full citation of the paper is: Verma NK, Dempsey E, Long A, Davies A, Barry SP, Fallon PG, Volkov Y, and Kelleher D (2012) Leukocyte function-associated antigen-1/intercellular adhesion molecule-1 interaction induces a novel genetic signature resulting in T-cells refractory to transforming growth factor-β signalling. Journal of Biological Chemistry.