People who have this disorder tend to have many other symptoms as well. They may have:
It is a disorder in which there is a general increase in symptomatology.
It depends. In clinical practice it has generally been an illness in which 90% of the people who are diagnosed with it were women.
In 2010 we changed the diagnostic criteria somewhat to eliminate one of the factors that might have led to this female predominance. That factor was pain on pressure.
When the examining physicians would touch people in certain areas, women would tend to complain of pain more than men.
This probably was related to a couple of things. One of which was related to the body habitus – women were generally smaller than men and less muscular.
Also human and animal studies have shown females have a decreased threshold for pain compared to males.
The change in criteria that occurred in 2010 eliminated this criterion. The consequence has been that studies that are beginning to be done tend to show that the prevalence of the disorder may be approaching 50% - that is to say the prevalence may be quite similar in women and men.
In the study that we just did there was only a very slight predominance of women.
Your recent research found that the prevalence of fibromyalgia in the general German population in 2012 was 2.4% and 1.8% in women and men respectively. Is this difference statistically significant?
Statistical significance is often a function of the size of the sample. So if instead of examining slightly more than 2,000 patients we examined more than 4,000 patients, that difference would have been statistically significant.
I think one can overplay the statistical significance in a study like this. That is why we tend to report things with confidence intervals which is another measure of how certain we are about the level we observe.
I would say that the prevalence is around 50:50 but it is probably more in women. I say that because other studies that have been done using survey methods have found a female predominance – but only a very slight predominance.
That is not entirely clear because what one sees in a population study might not be the same as what one sees in the clinic. Women tend to go to physicians more than men and so they’re more likely to be diagnosed than men.
In societal terms it may be more acceptable to have certain diagnoses if you are a woman rather than a man and vice versa depending on the situation.
So we have to be careful in extrapolating the results of this study to the clinic. In clinical studies of fibromyalgia, it has often been 90% women. Maybe the change in criteria will result in a change in diagnosis in the clinic but that remains to be seen.
How prevalent is fibromyalgia?
It is about 2%. Some countries will have slightly higher or lower percentages, but in general they will be around 1-5%. This is a high or low prevalence depending on perspective.
Fibromyalgia has been described as a spectrum disorder rather than a categorical illness. Please can you explain what this means and whether you agree with this statement?
What the results of our study showed is that we provided reasonably good evidence that fibromyalgia exists as a continuum rather than a dichotomous diagnosis.
A dichotomous diagnosis is a yes/no diagnosis. There are examples of this in medicine and in life. For examples:
- One has cancer or one does not have cancer
- The bone is either fractured or it is not
- There is an infection or not an infection
When we take a look at things such as hypertension (high blood pressure), we see that it is a continuous characteristic.
For example, taking the systolic number (the top number), blood pressures tend to go from 90 – 190. Somewhere along that line, groups have to decide that the value is abnormal.
Imagine they pick 140. If you have 141 you are hypertensive; if you are 139 you are normal.
There are obvious limitations to that, as the people at 139 and 141 are almost exactly the same. But there has to be a practical cut-off.
Those cut-offs are not made on the basis of disease, but they are made based on communities getting together and deciding which point is abnormal. For hypertension, the consequences of having high blood pressure might be heart attacks and strokes.
People decide if you get to a certain level it is serious enough that we think we should call it abnormal.
Recently, people have talked about reducing the cut-off for hypertension. So these are arbitrary cut-points.
In fibromyalgia, studies have shown that the symptoms of fibromyalgia exist on a continuum. From a little pain and a little distress: to a lot of pain and a lot of distress. In fact we call the measures that we use to diagnose fibromyalgia measures of polysymptomatic distress.
This is termed by the UK psychiatrist Simon Wesley who first described illnesses such as chronic fatigue syndrome and fibromyalgia being at the end of a continuum of polysymptomatic distress.
What do we mean by polysymptomatic? Many different symptoms. One might have headaches, but not have all of the symptoms of fibromyalgia.
To put it another way, people with fibromyalgia tend to have a lot of fatigue, a lot sleep disturbance and pain and symptoms and difficulty with thinking and functioning. So it isn’t just distress in one area, but it is polydistress.
You can think of polysymptomatic distress as a condition of humankind which represents both some people who have almost no symptoms and some people who have a major amount of symptoms.
Those who have studied fibromyalgia came up with a cut-point in which they said ‘this is sufficient symptoms to call it fibromyalgia and less than that is not sufficient’.
Although this may be helpful in the clinic, it is scientifically useless because we exist as a continuum.
One of the results of the study that we just did was to show that people who satisfy the fibromyalgia criteria in the general population often have very high levels of all of these characteristics and they satisfy this idea of a continuum.
This is an important point when thinking about some of the hypotheses about what causes fibromyalgia. Imagine we were talking about what causes high blood pressure and the issue was that you went from a blood pressure of 139 to 140. The idea of what causes something on a continuous scale is a much more complicated idea.
People who almost have fibromyalgia almost have it. So the idea that there are differences between people who have fibromyalgia and those who don’t have it is an idea which may not really be true.
The third thing we found in the study has to do with a new set of criteria that the psychiatrists are proposing in the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5). DSM-5 have created a condition that they call physical symptom disorder.
One of the issues that had come was whether people that had lots of symptoms should be classified in a book that measures psychiatric illnesses. There has been some discussion about all of this and we had the opportunity to make estimates on what population of people in the general population who had fibromyalgia would satisfy the new DSM-5 criteria. We came up with roughly 40%.
We don’t believe for a moment that these people have a mental illness. I think what we’ve shown is that there is a limitation about the way that DSM-5 looks at these sorts of conditions. There’s no real benefit to anybody to consider this in the way that DSM is considering it.
Our point is not really to argue one way or the other but just to provide information. This also touches on a long debated issue as to what constitutes a mental or a psychiatric illness. So when we mention this we are not mentioning it on the basis of showing that people have this sort of illness but rather that they fit these sorts of criteria. I don’t think the criteria are particularly useful. There’s also been a lot of general critique of the new DSM-5.
What we have done is provide data which will help people in the future make decisions on how to classify things. One could say that people who satisfy the fibromyalgia criteria also tend to satisfy the criteria for somatic symptom disorders, that gives us some additional insight into fibromyalgia.
Does the continuous nature of fibromyalgia make it difficult to diagnose?
Yes and no. It depends on how much fibromyalgia is present.
One of the problems with fibromyalgia is that people may be identified on the basis of behavioural symptoms. People who are having more pain or being more deliberate in demonstrating to observers that they have pain, or having more complaints that seem a little bit more severe, tend to be identified more easily as having fibromyalgia. Whereas, people who have the same disorder but aren’t as demonstrative about it may be missed.
There is a difficulty, but in clinical practice I think the question comes when people come and complain of multiple symptoms, the doctor has to make some sort of determination as to when they are serious enough to classify them separately.
Although we’ve had criteria for fibromyalgia for many years now – since 1990 – we know that these criteria are not really used in General Practice. Instead physicians tend to interview patients and listen to their symptoms and then make decisions based on the severity of the symptoms.
The new criteria that we developed in 2010 are based on the severity of symptoms. Although we suspect that physicians won’t use these criteria as strictly as we’ve written them, I think that they will tend to follow them.
Whether this is a legitimate way of looking at the illness is still in dispute. There are people who believe that this is an illness that is caused by underlying neurobiological abnormalities; there are other people that believe this illness represents a cultural illness – illnesses which have their basis in part in how society treats their symptoms and benefits and difficulties that are associated with them.
There are people who believe that this disorder has a predominant psychological basis. The underlying basis of this disorder is not entirely clear. One thing that is clear is that people who have these symptoms have severe distress.
We doctors may argue about the nature of the distress and what causes it, but there’s no question that people are very distressed by it and it may be a limiting problem.
How is fibromyalgia currently diagnosed and how do you think this method could be improved?
It is diagnosed right now by self-report on the basis of patients. Self-report is both good and bad. Self-reporting is inherently problematic. Inherently it has a degree of validity problems.
At the same time, self-reporting is very important. When I wake up in the morning with a headache, no one else knows I have a headache or how severe it is. Whether I choose to go to work or not go to work, it is based on the severity which is only known to me. So self-report is extremely important.
On the other hand, in illnesses such as fibromyalgia, this severity in the eye of the beholder may be problematic.
To diagnose fibromyalgia patients should:
- have pain in a number of areas of the body - widespread pain
- be substantially bothered by fatigue
- have difficulty in getting restful sleep
- often report problems with memory or thinking clearly
One problem that can arise from diagnosis is that people can gain disability benefits based on self-reported symptoms. Societies are not always certain as to how they should handle self-reported illnesses. This goes through all aspects of one’s life. People with fibromyalgia look healthy but they don’t feel healthy.
In the United States we have handicapped parking spaces, there are always letters to the editor of the newspaper saying they saw people park in the handicapped parking space and get out and look healthy. The idea that people have some of these disorders get benefits that are based on self-report.
The problem in self-reported illnesses is that the definition of illness is something that society needs to accept and verify as well. Some self-reported illnesses are not taken seriously. For example, people don’t take the illness Multiple Chemical Sensitivity very seriously. There are illnesses such as Recovered Memory Syndrome that was important as an idea in legal areas in the last decade.
These are illnesses that, regardless of what doctors do and don’t say about them, society has to give an OK about. Illnesses, such as fibromyalgia, tend to exist not just in the medical basis, there’s no microscope that finds the cancerous cell here, and it has in part to do with how society deals with this sort of thing.
The very wise and great Canadian historian Edward Shorter points out that the symptoms have to be legitimate in society. Some symptoms are allowed by society and some are not. The nature of what societies allow differs over time. The UK has had a great deal of problems over the years trying to decide what happens to fatigue syndromes, also known as ME. The issues in ME are the same as in fibromyalgia.
It is a complicated situation. Patient support groups, doctors, pharmaceutical companies, insurance companies, all have something to say about this sort of illness, so it is not an easy illness.
What is currently known about the causes of fibromyalgia?
The causes are controversial in a sense. Some of the best work in this area has been done by the UK groups. The UK groups have used validated epidemiological methods to study something called chronic widespread pain. This is one of the central characteristics of fibromyalgia.
What they found is that psychological features, childhood deprivation and features like that are determinants. Their work has been really very good. They have used some great UK data that was collected generations ago and they were able to get their hands on this data and find out what happened to the people.
They could then link childhood deprivation, trauma, sexual abuse and things like that. They found that people that had those things were more likely to develop widespread pain. We also know that familial depression is higher in people that have this sort of disorder.
On the other hand there have been recent advances in understanding what chronic pain is like within the brain in neurobiological systems. There have been proposals that something happens to the central nervous system in people who have this disorder and this change in the CNS makes pain chronic and is responsible for all of the symptoms one sees.
One has to go very far with that idea before it is really accepted. It is one of the major ideas of today.
The problem that we have with all of these ideas is that if one takes function magnetic resonance imaging (fMRI) of the brain of people who have fibromyalgia and compares it to normal people, one finds there are differences.
The problem with all this is that it is really in part the chicken and the egg, or cause and effect. If some terrible thing happened to your family for example and somebody said before you go anywhere get in this fMRI machine and let’s see what your brain looks like – I wouldn’t be surprised if they found abnormalities compared to normal people because that is the way that humans function – we all function through these neurobiological mechanisms and the fact that we see differences does not mean that the differences we see are the causes.
These are issues that people are studying on and working on right now. My own view is that there are many factors that produce these symptoms – some are psychological and some are physical and it does exist on a continuum.
Our ability as physicians to help people is to understand that everybody needs help regardless of whether they are symptomatic or distressed. Some people don’t need help and it exists on a continuum. Rather than oftentimes falsely finding our way into ‘this is sickness’ ‘this is health’ we should understand that symptoms exist over a continuum for humans and as physicians and healthcare workers everyone is entitled to good care and understanding – not just those who have the most severe symptoms.
If we take from fibromyalgia some of the distress that we see and realise that it exists in people who don’t quite meet the criteria and it is important to understand how they feel, we’ll have made important advances.
How far do you think we are from finding a cure for fibromyalgia?
If this is part of something that happens with mankind then maybe there won’t be such a thing as a cure. There are people who are anxious, people who worry a lot, there are some people whose personalities tend to be more down and depressive and others that tend to be happier. It is the nature of mankind to be that way.
The idea that they all have to be cured is a bad idea. We should not medicalise normal aspects of their lives. In any sort of situation we should help people that need help and perhaps we should leave people alone who don’t need help.
Currently what we’re doing with treatment for this disorder has not been very successful. The treatments that are most effective seem to be physical treatments such as exercise. Exercise helps people substantially.
Pharmacological treatments are less effective. In the United States we have 3 drugs that are approved for the treatment of fibromyalgia, in the European Community none of those drugs were approved because the regulators thought that the drugs didn’t work very well and they had hazards without benefits. Their studies of the drugs showed that the benefits were very minor.
My co-author on the study Dr Winfried Häuser has done the most important studies in understanding how effective or ineffective these drugs are and it is his work that I think is some of the most important work that has been done on this illness in the last decade.
Where can readers find more information?
We’ve recently started a website for physicians and health workers about fibromyalgia and it is called the Fibromyalgia Perplex: www.fmperplex.com
We just started the website a few weeks ago and it comes from A.A. Milne’s Winnie the Pooh. Specifically it comes from a title that Frederick Crews wrote in the 1960’s called the Pooh Perplex which was a take on academia.
Here we are trying to discuss some of the issues associated with fibromyalgia. Fibromyalgia in many respects has become a dominant theology. There has been enormous amount of pharmaceutical money, especially in the United States, on direct to patient advertising and sponsorship of groups.
In the US for example when you turn on the TV you can watch people advertising to patients about how much pain they had until they took these medicines. Then they say it is thought to be caused by over-reactive nerves.
There has been a large campaign to recruit people to the diagnosis of fibromyalgia. Remember that as a self-reported illness, people with pain often why they have it. The answer that often comes on the television ads is that you may have fibromyalgia and that there are drugs to help with it.
Fibromyalgia represents a dominant theology. There are others that say we would be better off if we just treated people instead of trying to make this into a disease which it is not.
In the medical literature, however, fibromyalgia is a well-established condition which has little opposition. I think it is important to recognise that the reason that there is little opposition in the medical literature is that you cannot write articles on a condition that you don’t think is a valid and useful entity.
If you ask physicians, and there are many studies like this in Canada and the UK, about how they think about illnesses like this. There is a lot of doubt about how doctors feel about this as a separate illness.
A study published a year ago in the UK by Gareth Jones looked at whether or not trauma could cause chronic widespread pain. This is a very important issue because for example if you are in the US and you are in an automobile accident and you have symptoms that are alleged to be fibromyalgia, this is where you can see the reported symptoms might be a bit of a problem, the question is whether the trauma caused the fibromyalgia. There have been very extensive lawsuits – there is a whole legal industry that has been developed that surrounds this particular issue.
Gareth Jones did this wonderful study where they got people who did not have widespread pain and they followed them and they saw which people developed widespread pain and they looked at the role of trauma. It seems as if motor vehicle accidents were associated with the development of chronic widespread pain.
Then they analysed the data on the basis of baseline characteristics and they found that if you adjusted for the baseline psychological characteristics of the people in the study that this difference disappeared.
The meaning of this was that the trauma itself for the most part didn’t cause fibromyalgia but the characteristics of the people played the important role.
These kinds of studies are very important for understanding the nature of the illness, but they also show what the problems are.
One thing to note is that the severity of the trauma, at least according to current observations, isn’t necessarily thought to be so important. One idea is that if you have trauma it may disturb you and cause mental stress which may then cause fibromyalgia.
Without saying whether that is correct or incorrect you can see how that may cause a problem within societies and in courts and in governments – knowing how to handle these sorts of things. So fibromyalgia turns out to be a very complicated problem.
What our study did was to take out these issues and just look at a population of people and 97-98% didn’t have fibromyalgia. Out of that we were better able to understand some of the characteristics as people didn’t need to worry about being sick or being well and answering these questions.
The famous American author and physician Nortin Hadler wrote that if you had to prove you were sick, you couldn’t get better!
In the United States for example suppose you got injured and you tried to get compensation for your injury, if you got better you don’t get compensation so you have to stay sick. You have to convince people that you are really ill and it’s a system that creates substantial problems.
These are not easy problems and they have been around for long periods of time. In fact you can find evidence of fibromyalgia that goes back well into the 19th century and up until the mid-1920’s in an illness that was called neurasthenia which looks almost exactly the same in many of its aspects as fibromyalgia.
So fibromyalgia is a social illness, it’s a societal illness, it’s a personal illness it has social consequences for patients and doctors and financial consequences that are worth a lot of money for pharmaceutical consequences, it is worth a lot publications to physicians. There is a lot invested in what I would
call a psycho-cultural illness.
About Dr Frederick Wolfe
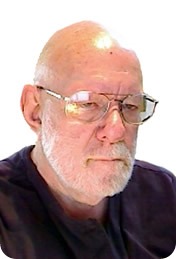 Dr. Wolfe is Clinical Professor of Medicine at the University of Kansas School of Medicine – Wichita, and Director of the National Data Bank for Rheumatic Diseases.
Dr. Wolfe is Clinical Professor of Medicine at the University of Kansas School of Medicine – Wichita, and Director of the National Data Bank for Rheumatic Diseases.
He received his medical degree from the State University of New York, Downstate Medical Center, and completed medical residencies at the Downstate Medical Center and the University of Kansas Medical Center.
The author of more than 400 scientific articles, he received 1995 Distinguished Rheumatologist Award of the American College of Rheumatology (ACR), and was elected as a Master of the ACR.
He was the senior author of the 1990 and 2010 ACR classification criteria for fibromyalgia.
He is author of numerous papers on the longitudinal outcomes of rheumatoid arthritis, including work disability, functional disability, psychological status, mortality, and the effect of treatment on rheumatic disease outcome.
His current work involves the use of patient and physician data banks to understand the outcomes of rheumatic diseases.