Molecular Breast Imaging (MBI) is a highly effective secondary diagnostic tool, particularly for women with dense breast tissue.
Studies have shown that mammograms fail to detect cancers in one-third to one-half of women with dense breasts (Clinical Literature on MBI). In some cases, the findings from a mammogram are inconclusive and secondary screening will almost always be required.
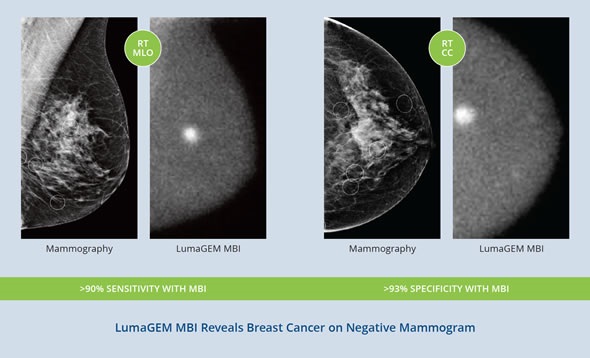
Even with negative results for women with dense breast tissue (or who are considered high-risk for breast cancer), an adjunctive MBI test should be considered.
Dense Breast Patient - LumaGEM MBI Results Review
How is breast density measured and how many women are thought to have dense breast tissue?
Currently right now, providers use The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) scoring method using a 1-4 rating system.
This classification system allows radiologists to measure and describe breast density
- BI-RADS 1 : <25% Dense Breast Tissue
- BI-RADS 2 - 26-50% Dense Breast Tissue
- BI-RADS 3 – 51- 75% Dense Breast Tissue
- BI-RADS 4 - >75% Dense Breast Tissue
Nearly half of all women in the United States have dense breast tissue. From the advocacy group areyoudense.org, some simple facts about women with dense breast tissue:
Five facts about dense breast tissue
- 40% of women have dense breast tissue
- Breast density is one of the strongest predictors of the failure of mammography to detect cancer
- Mammography misses every other cancer in dense breasts
- Breast density is a well-established predictor of breast cancer risk
- High breast density is a greater risk factor than having two first degree relatives with breast cancer
Why can mammograms sometimes fail to detect cancers in women with dense breasts? How often is this thought to occur?
Digital mammography is the golden screening standard to detect early breast cancer. Mammography is effective and with our screening protocols, it is a major reason for the decrease in mortality. However, the ability of mammography to detect breast cancer in women with dense breast tissue is limited.
The dense breast tissue hinders the ability to detect cancer. Acting like a white cloud, the dense breast tissue becomes more white, the denser the breast. Women with primarily fatty breasts will have a mammogram that appears darker. The “white” artifact limits the ability to see and identify cancers.
In general approximately 10-20% of breast cancers are missed by standard mammography – that percentage can approach 40-50% in women with dense breast tissue.
The issue of breast density is important.
Why are the findings from mammograms sometimes inconclusive?
Dense breast tissue and its ability to mask what needs to be seen is sometimes why mammograms are inconclusive. Traditionally if the patient has incomplete or abnormal findings on a mammogram, the radiologist would recommend for further examinations. This would include additional mammogram views, an Ultrasound or an MBI or MRI scan.
How does MBI detect lesions in dense breasts?
Compared to structural anatomical imaging, molecular functional imaging enables and improves quantitative measurements of physiologic function assessments of molecular pathways, both in healthy and in diseased tissue.
In other words, rather than seeing the anatomical views/structures of the breast, what MBI does, is image the functionality of the tissue. If a tumor is present, uptake of the radiotracer will increase around the area of interest and the image will display the concentrated uptake.
How does MBI compare to other secondary diagnostic tools?
As a secondary diagnostic tool, MBI has distinct advantages over ultrasound, MRI and 3D mammography (tomosynthesis):
- Non-automated ultrasound is operator dependent with low resolution and sensitivity. In general, whole breast ultrasound has low sensitivity and increased false positive findings.(1)
- The addition of breast MRI to mammography may result in a higher cancer detection yield, but findings have also demonstrated an increased number of false positive biopsies.(2) In addition, many women are not candidates for MRIs because of pacemakers or other ferromagnetic implants, poor renal function, claustrophobia, and body size or gadolinium allergies.
- 3D mammography may provide slightly higher specificity when compared to mammography (64% vs 60%); however, it does not match specificity rates of MBI or MRI.(3) MBI specificity was reported as high as 93% following mammogram.(4)
What do you think the future holds for MBI?
In the coming year of two, we expect adoption of MBI to spread and for the American College of Radiology to issue practice guidelines for the utilization of MBI, which will further accelerate its adoption.
With healthcare delivery changing in the United States, costs and patient outcomes are becoming more and more important to clinicians, providers, payers and patients. We believe that this emphasis will promote a critical assessment of breast cancer detection practices and drive the pursuit of protocols that will aim to improve patient outcomes (i.e., find more cancer earlier) at a lower cost.
In fact, a recent study by Milliman, a healthcare actuarial firm, found significant variation in diagnostic screening practices (https://www.milliman.com/en) and highlights the need for broadly accepted practice protocols to drive patient outcomes and reduce costs.
The healthcare economic trends, combined with the grassroots advocacy for breast density awareness are driving higher patient involvement in their breast cancer screening decisions and increasing the demand for secondary medical imaging to screen for breast cancer. These two trends will in turn result in healthcare providers and clinicians to evaluate their screening practices and, ultimately, accelerate the adoption of MBI.
What are Gamma Medica’s plans for the future?
Our plans are to continue promoting the benefits of MBI to women with complex breast anatomy, including breast density, and educate the marketplace in order to support our market leadership.
As market adoption accelerates, we expect to see our business grow and prosper while fulfilling our mission of helping more women, and their families, avoid the health challenges associated with late stage breast cancer.
Our bottom line is to enable physicians to save more lives of the over 28 million women in the U.S. who might otherwise not benefit from routine mammography screening.
Where can readers find more information?
Gamma Medica, Inc. is dedicated to the development of advanced digital imaging technologies that address the growing importance of overcoming the critical shortcomings of mammography and other screening modalities in the early detection of breast cancer.
The company designs, builds and services the LumaGEM® MBI system, the first commercially available, FDA-cleared planar, dual head, fully solid-state digital imaging system utilizing cadmium zinc telluride (CZT) technology for molecular breast imaging.
For more information, visit www.gammamedica.com. Or follow us on Facebook, Twitter (@gamma_medica).
About Jim Calandra
 Jim Calandra, President and CEO, has over 20 years of management experience in the healthcare industry as an officer and director of several healthcare companies.
Jim Calandra, President and CEO, has over 20 years of management experience in the healthcare industry as an officer and director of several healthcare companies.
Prior to joining Gamma Medica, he was a founding partner of Birch Hill Partners, LLC, a management consulting firm specializing in advising private equity portfolio companies.
In particular, Jim is recognized for his expertise in strengthening the financial position, strategic direction and management of rising stars in the technology field.
Jim brings strong corporate governance, operational and financial management experience to his position as president and CEO of Gamma Medica. Jim has a BS and an MS in Accountancy from Bentley University. He is also a certified public accountant licensed in the Commonwealth of Massachusetts.
References
- Wendie A. Berg, MD, PhD Zheng Zhang, PhD, Daniel Lehrer, MD, et al. Detection of Breast Cancer With Addition of Annual Screening Ultrasound or a Single Screening MRI to Mammography in Women With Elevated Breast Cancer Risk. JAMA, April 4, 2012—Vol 307, No. 13
- Berg WA, Zhang Z, Lehrer D, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012; 307(13): 1394-1404
- GurD, Abrams GS, Chough DM, et al. Digital breast tomosynthesis: observer performance study. AJR. 2009; 193:586-591
- Boyd NF, Dite GS, Stone J, et al. Heritability of mammographic density, a risk factor for breast cancer. NEJM. 347:886-894.