The number of blind people is high. In 2010, the World Health Organization estimated that, throughout the world, approximately 39 million people are blind. We understand the real size and meaning of this number if we consider that, of these, 80%, i.e. 4 out of 5 could be avoided, either by treatment or by prevention.
9 out of 10 avoidably blind people live in low-income countries. They become blind because they are out of reach from eye care. In other words, the core issue lies in linking up patients with eye care providers.
As an example, consider Kenya. For a population of 40 million people, there are just over 80 practicing eye doctors. With these numbers, the only way to ensure that people have access to eye care is to go out in the community, and screen within the community itself for patients who need to be referred to a specialist.

Please can you give an introduction to Peek and explain how the technology differs from traditional eye examinations?
Mobile phones are used even in the remotest parts of the world. Peek is a comprehensive set of high-quality eye tests entirely implemented on a smartphone. It consists of an app, and of a small plastic adapter, Peek Retina, that clips on the phone.
It has been designed by a consortium that includes the University of Strathclyde and the National Health Service Scotland, in Glasgow, and the London School of Hygiene and Tropical Medicine, and it enables community workers with minimal eye care training, such as school teachers or village chiefs, to identify patients directly within their communities, and to link them to eye care. In this, it assists traditional eye care by providing the missing link between patients and healthcare.
What factors were taken into consideration when designing Peek and what challenges needed to be overcome?
Peek is designed to be used by community workers with minimal training. For this reason, the Peek team has re-engineered the eye tests so that they can be performed correctly with the assistance of simple instructions on the phone screen.
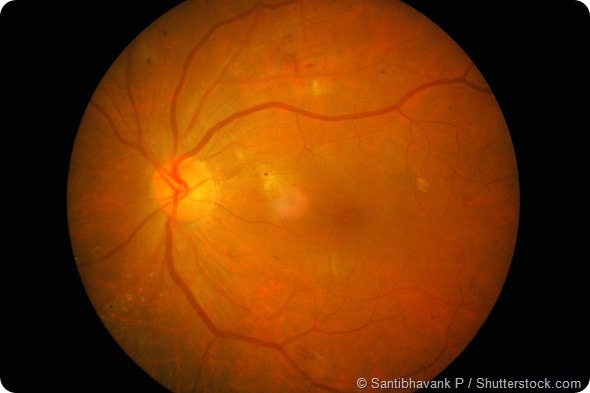
Furthermore, in order to visualize the back of the eye, we have invented Peek Retina, an inexpensive adaptor made of simple plastic parts that allows taking photographs of the retina with extreme ease of use.
Also, we have designed Peek to maintain the look-and-feel of a mobile phone. This links the test experience to a friendly and familiar everyday object. This is extremely important to ensure acceptance by the patients.
Does the sight simulation tool help to communicate with the patient and their family?
Indeed, once a community worker has measured the visual acuity of a patient, Peek uses a technology invented by the Sight-Sim group in Glasgow (http://www.sight-sim.co.uk/) to take the video stream from the camera and to simulate on the phone screen the blur seen by the patient. This can provide significant help in managing patients with low vision.
For example, by showing a schoolteacher the blurred images seen by a student, the teacher can understand the difficulties experienced by the child, and provide them with a thicker pen, thus avoiding the vision problem becoming a learning problem.

Can you please explain how the retina adaptor works?
The Retina adaptor is a small and inexpensive plastic clip that attaches onto the phone camera. It has a tiny optics that allows the phone to shine light through the pupil onto the back of the eye, and the phone camera to see the back of the eye. With Peek Retina, the operator can therefore take photographs of the back of the eye, as easily as taking a snapshot.
What impact do you think the retina adaptor will have on eye examinations?
Looking at the back of the eye is an essential medical examination. At present, devices that allow this are either extremely expensive or very difficult to use. With the Peek Retina adaptor, this essential test can be performed in the community, by community workers, thus allowing a better, more effective screening for eye disease.
Furthermore, the need for screening of the back of the eye exists also in high-income countries, such as the UK, for socially significant diseases such as diabetes, or as part of the admission process in Accident and Emergency Departments. Further applications are in general practice, or as part of medical training. Peek Retina has therefore the potential to become an invaluable tool globally.
Please can you outline the research that has been carried out so far using Peek?
Peek is being trialed in many countries. Studies are ongoing or planned in Kenya, Malawi, Mali, Tanzania, Botswana, India, Madagascar, UK, and more. In a recent study, the Kenyan Peek collaborators have liaised with a group of local schools, and the schoolteachers have screened more than 20.000 children in 9 days. This clearly shows the potential of this technology.
What do you think the future holds for eye examinations and portable kits?
Throughout the world, life expectancy is increasing, and older people tend to require more healthcare. This has two implications. The first, is that as many healthcare interventions as possible need to shift from hospitals to family doctors, to healthcare community workers and to the community itself.
The second, is that focus needs to shift from treating illness to maintaining wellness. In both these aspects, portable and inexpensive technology is key. Importantly, as these issues are global, and affect both high- and low-income countries, the more we leverage on globally pervasive technology, such as mobile phones, the more we contribute to reducing inequality in healthcare.
Where can readers find more information?
The Peek project website is www.peekvision.org, where it is possible to have a snapshot of the current state of the project and to register for updates. Our Twitter feed is @peekteam.
About Dr Mario Ettore Giardini
Electronic engineer and computer scientist by training, Dr Giardini works on the frontier between optics, electronics, and medicine.
In 1997 he has joined as Research Scientist the Italian National Institute for Physics of Matter (INFM). From 2005 to 2008 he has moved to industry, heading the R&D Division of a leading European microscope manufacturer, interacting closely with Asian Industry and industrial R&D.
He currently holds a Lectureship in Digital Health at the Department of Biomedical Engineering of the University of Strathclyde, in Glasgow, UK, where he explores technologies for field and mobile medicine, for virtual reality enabled healthcare and for medical robotics. Devices and instruments derived from his research are sold worldwide.