“Genomic medicine really needs deep learning,” these were the words of keynote speaker Brendan Frey, CEO Deep Genomics at RE-WORK’s Deep Learning in Healthcare Summit 2016.
Frey outlined the main issue blocking genomic medicine, the Genotype-Phenotype Gap, through a novel quotation from Eric Lander:
Genome.
Bought the book.
Hard to read.”
This quotation was taken from 2004, but the gap between the ability to collect genetic data and understand it’s meaning in a reliable, scalable and trustworthy way is one that we still haven’t managed to fill.
Frey’s hope is to use deep learning to close the Genotype-phenotype Gap through superhuman artificial intelligence, for humans themselves have so far been unable to fully understand the genome.
_thumb.jpg)
Brendan Frey, President & CEO, Deep Genomics
Resorting to AI may sound like something from science fiction, but computer programs with superhuman abilities have become reality with Google DeepMind’s recent success in beating a professional player at the game of Go.
Professor Neil Lawrence, University of Sheffield, however, is disappointed it took so long for deep learning to crack the game of Go, particularly when computer programs were able to beat humans at Chess over 20 years ago. Lawrence described the data delusion and the current inefficiencies of deep learning in terms of the tools used.
“The tools you use shouldn’t limit the way you think”, however, was the key principle of Diogo Moitinho de Almeida, Senior Data Scientist, Enlitic, who believes we can do better and that “deep learning is awesome.”
Some of the applications of deep learning at the Summit certainly did seem awesome. Ali Parsa, CEO of Babylon Health demoed their upcoming app which asked the user a series of questions in order to determine the severity of the user’s medical symptom, in the same way as a triage nurse. Parsa hopes that deep learning can even take us one step further from sickcare to healthcare.
The move towards a more predictive rather than reactive healthcare system was also discussed during a panel on how AI will help to enhance and personalize healthcare. Cosimo Gretton, a doctor at Guy’s and St Thomas’ NHS Foundation Trust described how predictive analytics in healthcare is a transformative approach but it will require changes to the system so that clinicians can use the algorithms successfully.
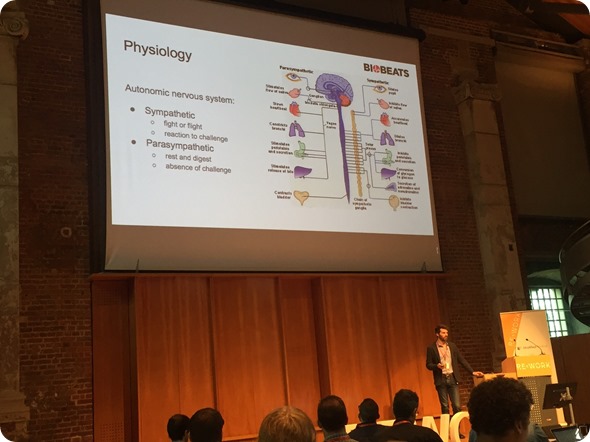
Davide Morelli, CTO, Biobeats
Gretton also described how AI can enhance the skills at each stage of the healthcare chain, from patients to healthcare professionals. Using AI to take control of our own health was also a strong theme in Davide Morelli’s talk. The CTO of Biobeats outlined the physiological response to stress in terms of the sympathetic and parasympathetic nervous systems. Morelli went on to explain how deep breathing using the diaphragm can trigger the vague nerve and thereby force the user to calm down. This deep breathing technique can now be learnt via Biobeats’ ‘Hear and Now’ app, which tracks a user’s heart rate to see if they are successfully using their diaphragm when deep breathing and gives immediate biofeedback so a user can learn on their own.
Tracking heart rate variability through a health sensor was also a key part of Daniel McDuff’s talk. The Director for Research at Affectiva, outlined how webcam images have been used to train algorithms to detect a physiological response, more specifically photoplethysmography (PPG), traditionally measured through skin contact.

Daniel McDuff, Director of Research, Affectiva
McDuff outlined a collaboration with Brigham and Women’s Hospital to try to use the technology to help people with peripheral artery disease. Affectiva’s technologies based on deep learning may also be used for suicide risk assessment by measuring facial expressions.
Medical image computing certainly seems to be an area where a lot of progress has been made. Ben Glocker, Lecturer at Imperial College London, described the advances in machine learning in terms of intelligent imaging such as building models of foetal brain development. The challenge he highlighted, however, was to make use of unlabelled data for unsupervised learning.
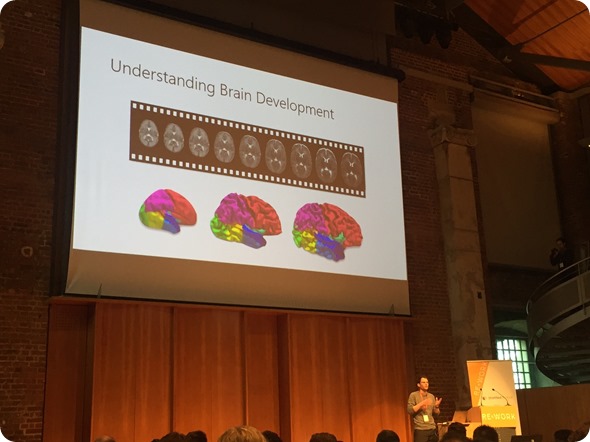
Ben Glocker, Lecturer, Medical Image Computing, Imperial College London
Data is certainly a big issue. Michael Nova, Chief Innovation Officer, Pathway Genomics reminded us of IBM Watson’s prediction that medical data will double every 73 days by 2020 and it already doubles every 3 years.
Further shocking statistics came from Alejandro Jaimes, CTO and Chief Scientist of AiCure who highlighted how bad we are at taking medicines, with ~50% of people not taking their medicines as prescribed. Even more worryingly, Jaimes expressed that failing to follow prescriptions causes about 125,000 deaths in the US alone.
AiCure’s smartphone app hopes to help solve the adherence problem, both in population health and clinical trials, where it is thought that ~ 43-78% of participants don’t take their medicines as prescribed. The app uses the phone camera to autorecognise the person’s face, pill and action of taking the medication. The app has also learn to detect fraud through spitting and other abnormal behavior detection to catch participants trying to cheat.
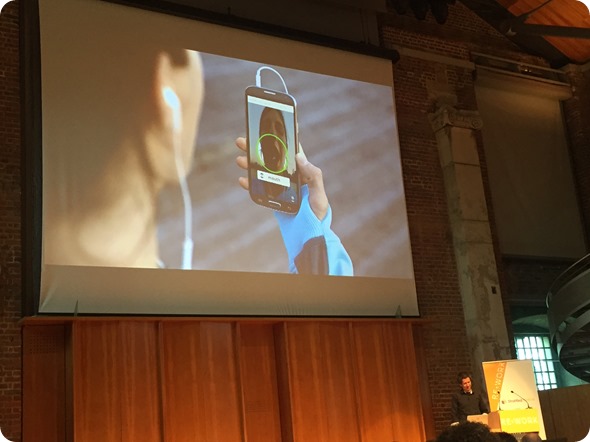
Alejandro Jaimes, CTO & Chief Scientist, AiCure
In addition to improving healthcare with current medications, the RE-WORK Summit focused on the role of deep learning in developing new medicines. Jackie Hunter, CEO of Stratified Medicine, highlighted her optimism that deep learning can help change the drug discovery paradigm. Through augmented intelligence, Hunter advocated the production of fewer molecules but the right molecules, thereby creating a leaner drug discovery model.
Ultimately, current models aren’t working in many aspects of healthcare, from the costly nature of present drug discovery to the exponential data problem of personalized healthcare, so perhaps it is not just genomic medicine that really needs deep learning, but healthcare as a whole.

Michael Nova, Chief Innovation Officer, Pathway Genomics
Source: RE-WORK Deep Learning in Healthcare Summit