IBS is a common medical condition which is diagnosed in the presence of characteristic gastrointestinal symptoms including recurring bouts of abdominal pain and diarrhea and/or constipation. IBS patients also commonly report bloating and abdominal distension or swelling.
Two thirds of IBS patients associate symptom onset or worsening with eating a meal. IBS affects between 7-15% of the US adult population and adversely affects quality of life and work productivity.
Not surprisingly, IBS exacts a significant personal toll on sufferers and causes a significant financial burden to the health care system and society.
How much is known about the causes and triggers of IBS?
Though patients with IBS are bound together by similar symptoms, the causes of symptoms can vary from person to person.
Research has shown that IBS patients often have abnormalities in the function and sensation of the intestines and colon. Abnormalities have also been identified in the way that the brain and the nervous system in the GI tract interact – so called abnormal brain-gut interactions.
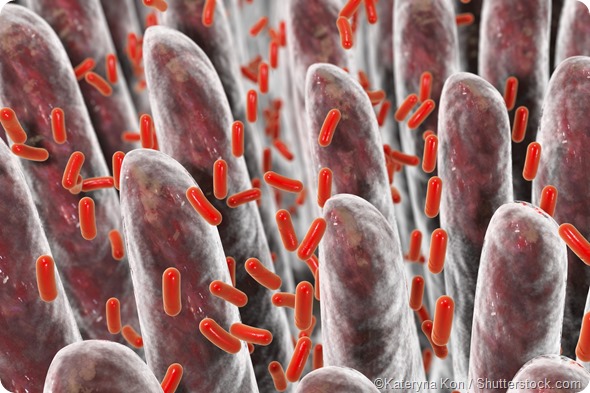
Recent work has found that the bacterial living in the GI tracts of IBS patients are altered when compared to healthy persons. Changes in the permeability or leakiness of the lining of the GI tract as well as activation of the immune cells lining the GI tract have been found in some IBS patients.
A severe infection of the GI tract (food poisoning or traveller’s diarrhea) increases the risk of developing IBS – perhaps by altering one or more of the mechanisms outlined above.
As already mentioned food is a common trigger for IBS symptoms. Medications like antibiotics and other types of drugs which affect the function of the GI tract can also trigger IBS symptoms. Stress or anxiety are also known to be important triggers for IBS.
Are certain foods responsible for IBS symptoms?
Two thirds of IBS patients report that their symptoms are triggered or worsened by food. IBS patients with food related symptoms have worse quality of life than IBS patients who symptoms are not food related.
Though the types of foods which trigger symptoms vary from person to person, survey studies suggest that symptoms are most commonly triggered by carbohydrates. Fatty foods can cause problems for some IBS patients.
Many IBS patients associate their IBS symptoms with eating wheat or dairy products. Though wheat and dairy certainly contain carbohydrates which some persons have difficulty digesting or absorbing and thus, can get to the colon where they are fermented to produce chemicals called short chain fatty acids and gases which can trigger IBS symptoms, these food sources also contain proteins (for example gluten and casein) which could also lead to symptoms through activation of the gut immune system.
While true food allergies are relatively rare in adults with IBS, it is possible that certain proteins could abnormally activate the immune system in the GI tract leading to changes in function and sensation that could lead to symptoms in IBS patients.
Do triggers vary widely from person to person?
While IBS patients most commonly associate symptoms with eating carbohydrates, strategies like the low FODMAP diet which restricts the intake of poorly absorbed carbohydrates leads to symptom relief in roughly half of IBS patients.
Though this is quite encouraging, it is clear that many IBS patients with food-related symptoms are not adequately served by the low FODMAP diet. This fact speaks to the importance of considering other dietary triggers of IBS symptoms and further research to develop diagnostic tests and novel dietary interventions for IBS patients.
Traditionally, what method has been used to identify trigger foods?
Most of the dietary strategies utilized in clinical practice for IBS are empiric – in other words, symptoms are determined to be food-related and then the health care provider along with the patient, typically based upon their previous experiences and knowledge, choose a diet to try like a gluten free diet or the low FODMAP diet.
The choice of diet intervention or foods to eliminate are currently not commonly driven by diagnostic testing – largely because there is little high quality research to support the use of available tests to identify food triggers in IBS patients.
Some have tried to use food diaries to identify food triggers but unfortunately, the use of traditional hand-written diaries has not proven to be a reliable or accurate means of identifying food triggers in IBS patients.
What developments have been made in the identification of foods that trigger IBS symptoms?
There is interesting work which hopes to identify novel testing strategies for IBS patients with food intolerances. For example, if one believes that certain dietary proteins can abnormally activate the gut immune system, it is possible that antibodies to offending proteins might be measured in the bloodstream.
It might also be possible to leverage the gut microbiome or the metabolic consequences of alterations in the microbiome to identify IBS patients who are more or less likely to respond to specific diet interventions.
These novel lines of research open the door to the possibility of moving from the current trial and error approach to a more objective, personalized approach to choosing the optimal diet therapy for each IBS patient.
What further research is needed to evaluate the developed tests?
Though the association between IBS and food has been clear for quite some time, research to understand this association is in its infancy. Much work is needed to identify the right targets, also called biomarkers, which should be tested in large clinical trials.
I would caution health care providers and patients from putting too much faith in reports of tests conducted in small numbers of patients. The road is paved with tests and treatments which appeared ground-breaking in small, poorly designed clinical studies only to be found ineffective when subjected to the scrutiny of a large, properly designed clinical study.
What do you think the future holds for patients with IBS?
The future will bring the development of biomarkers which will allow health care providers to separate IBS patients on the basis of pathophysiology as opposed to symptoms alone. This will allow us to offer a more precise explanation for the cause of symptoms in IBS patients.
The importance of this statement should not be underestimated as IBS patients are currently told that they have a disorder, not a disease, the cause of which is unknown, will last a lifetime, and for which there is no cure.
The imprecision and fatality of this explanation for IBS is typically disconcerting and robs hope from affected sufferers. Perhaps even more importantly, the identification of reliable biomarkers might allow us to choose the most appropriate therapy for each individual patient with IBS.
Are there additional IBS triggers other than food that can be tested for?
There is a new diagnostic test available in the US called IBS-Chek. This test identifies the presence of anti-cytolethal distending toxin B and anti-vinculin antibodies which appear following certain bacterial gastroenteritis infections.
In healthy persons, these antibodies are only present for a short time around the acute infection. In IBS patients, these antibodies persist and studies show that the presence of these antibodies can distinguish between IBS patients, healthy controls, and patients with Crohns disease, ulcerative colitis, and Celiac disease.
Other diagnostic tests which identify abnormalities in the handling of bile acids in the GI tract are also under development and might allow the identification of IBS patients more likely to respond to treatments aimed at bile acids.
As already mentioned, there are also groups working to better understand the gut microbiome and metabolomics and how they might be leveraged to develop new diagnostic tests which will help health care providers to choose the right therapy for the right patient.
Where can readers find more information?
Our websites provide information about food and GI symptoms and specific information about the low FODMAP diet:
A few scientific papers of interest:
- Chey WD, Kurlander J, Eswaran S. Irritable Bowel Syndrome: A clinical review. JAMA. 2015;313(9):949-958.
- Spencer M, Chey WD, Eswaran S. Dietary renaissance in IBS: Has food replaced medications as a primary treatment strategy? Curr Treatment Options Gastroenterol 2014;12:424-440.
- Chey WD. David Sun Lecture: Food - The main course to health and illness in IBS. Am J Gastroenterol 2016;111:366-71.
About Dr Bill Chey
William D. Chey, MD, AGAF, FACG, FACP, Scientific Advisor, Biomerica Inc., Timothy T. Nostrant Professor of GI & Nutrition Sciences, Director, GI Physiology Laboratory, Director, Digestive Disorders Nutrition & Lifestyle Program, Medical Director, Michigan Bowel Control Program, President, Clinical Excellence Society, Division of Gastroenterology, University of Michigan Health System, Ann Arbor, MI, USA.
 Dr Chey received his BA degree from the University of Pennsylvania and medical degree & training in internal medicine at the Emory University School of Medicine. He completed a fellowship in gastroenterology at the University of Michigan in Ann Arbor.
Dr Chey received his BA degree from the University of Pennsylvania and medical degree & training in internal medicine at the Emory University School of Medicine. He completed a fellowship in gastroenterology at the University of Michigan in Ann Arbor.
Following fellowship, Dr Chey has remained at the University of Michigan, where he is currently Timothy T. Nostrant Professor of GI & Nutrition Sciences.
He has helped to found and directs a number of programs at the University of Michigan including the Digestive Disorders Nutrition & Lifestyle Program and Michigan Bowel Control Program.
His research interests focus on the diagnosis and treatment of the functional bowel disorders, acid-related disorders, and Helicobacter pylori infection. Dr Chey has received funding for his research from federal and private sources.
He is a medical innovator with 4 patents to his credit. Dr. Chey is co-founder and chief medical officer of My Total Health, a health information technology start-up.
Dr Chey has authored more than 300 manuscripts, reviews and book chapters. He is Editor Emeritus of the American Journal of Gastroenterology (2010-2015) and Clinical & Translational Gastroenterology (2011-2014).
Dr. Chey is a member of the Board of Trustees of the American College of Gastroenterology. Dr. Chey joined the Board of Directors of the Rome Foundation in 2010 and is a member of the editorial board of the Rome IV criteria.
In 2016, he was elected to the Council of the American Neurogastroenterology & Motility Society. He is a member of the Advisory Board of the International Foundation of Functional GI Disorders.
He has been elected to “Best Doctors” since 2001, “America’s Top Doctors” since 2009 and has repeatedly been recognized as a “Top Doctor” by Hour Detroit Magazine. In 2015, Dr. Chey was named as one of the “190 Gastroenterologists to Know” by Becker’s ASC. In 2016, Dr. Chey was named to Helio magazine’s: Helio 200, a list of key opinion leaders and innovators in Gastroenterology & Hepatology.
In 2014, Dr. Chey was inducted into the Department of Internal Medicine’s Clinical Excellence Society of which he now serves as President, received the Dean’s Outstanding Clinician Award, and was inducted into the League of Research Excellence at the University of Michigan.
In 2015, he was inducted into the League of Clinical Excellence at UM and received the Distinguished Clinician Award from the American Gastroenterological Association.