Feb 17 2017
Three-quarters of those who describe their disease as moderate to severe say their disease is ‘poorly controlled’, with a third having had five or more flares over the past year
New research shows that nearly three-quarters of patients with moderate to severe ulcerative colitis (UC) taking conventional treatments describe their disease as ‘poorly controlled’ (continuous or regular experience of symptoms that negatively affect quality of life), with half saying they are somewhat or completely dissatisfied with their current medication; only 1% were completely satisfied with their current treatment.
Ulcerative colitis is a chronic disease, causing inflammation and ulceration of the inner lining of the rectum and colon (large bowel), and is one of the two most common forms of inflammatory bowel disease ̶ the other is Crohn’s disease. The research was commissioned and funded by MSD with the co-operation of Crohn’s and Colitis UK, who provided a link to the survey via its website and social media channels.
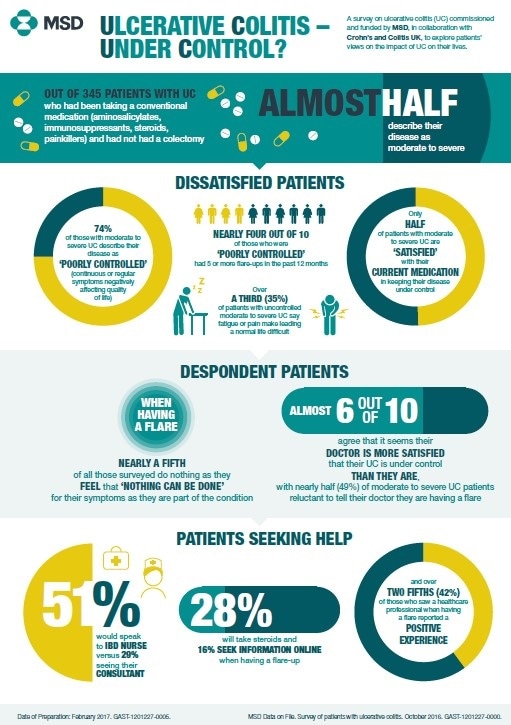
A third of those with moderate to severe UC reported experiencing five or more flare-ups over the past 12 months. Symptoms during flare-ups negatively affect patients’ quality of life, and include frequent bowel movements, blood in stools, high temperature, stomach pains and fatigue.
Dr Charlie Murray, Clinical Director of Gastroenterology at the Royal Free Hospital, London, says:
Despite advances in therapy and a better understanding of disease, these results demonstrate that we need to do better in managing ulcerative colitis and that we should always be aiming for full symptom relief.
The online survey considered the level of disease control, satisfaction with treatment and impact on quality of life among 345 adults with ulcerative colitis who were biologic-naïve, non-colectomised and currently taking conventional therapies. As this research was not accompanied by physician assessment, there are limitations on drawing conclusions from patients’ feedback. Of the 345 respondents, 162 (47%) described their symptoms as moderate (symptoms are bothersome) or severe (symptoms interfere with normal activities). Just under half (48%) of all respondents were aged 25–39, 29% were aged 40–54 and 10% were aged 24 and under; and three-quarters (75%) were female.
Low expectations, high despondency
Patient expectations of effective intervention when experiencing a flare are often low, with a fifth of patients taking no action as they feel ‘nothing can be done’ for their symptoms. Of all those surveyed, 41% are reluctant to report flare-ups to their doctor, and 59% of all patients believe their doctor is more satisfied that their UC is under control than they are, suggesting a significant degree of resignation and despondency that prevents people with UC seeking help. However, of those who did see a healthcare professional when having a flare nearly half (42%) were positive, stating they had a satisfactory experience, were offered good support and that their IBD nurse was easily contactable.
When patients do contact a healthcare professional, the survey found they are more likely to speak to an IBD nurse than a consultant – 51% would speak to an IBD nurse and 29% would visit their consultant. A proportion of patients would not seek advice from a healthcare professional at all – 28% take steroids during a flare, and 16% look for help and information online.