An interview with Professor Willie Hamilton, conducted by April Cashin-Garbutt, MA (Cantab)
Why can it be difficult, particularly in young people, for GPs to distinguish between patients with non-serious conditions, such as IBS, and serious conditions, like bowel cancer and inflammatory bowel disease?
The fundamental problem is that the symptoms are very similar, or at least some are. Taking your example of IBS – this is characterised by abdominal pain, plus sometimes diarrhoea or constipation. Yet these are key symptoms of abdominal cancer!
Taking a more ‘alarming’ symptom such as rectal bleeding – this is incredibly common too, with benign causes like piles, far more likely than cancer of inflammatory bowel disease (IBD).
Add in the relative rarity of cancer in the young – most GPs won’t see a case under 40 in their career – and you have a perfect storm!
Can you please introduce the new tool aiming to support GPs to identify the symptoms of a serious bowel condition in patients under 50 years old?
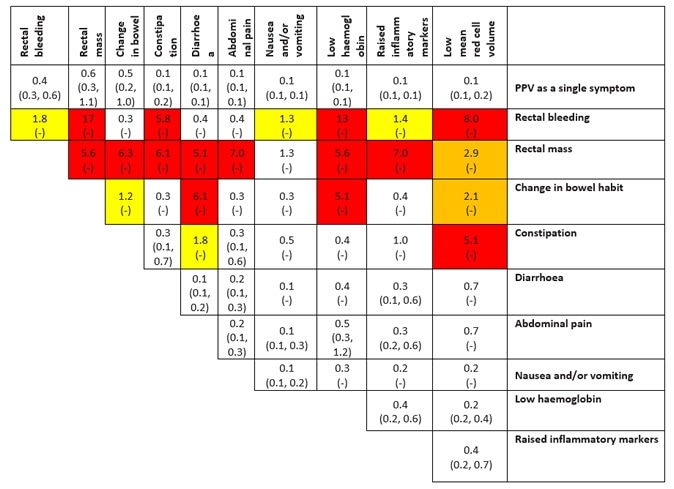
It gives the risk of serious disease (i.e. cancer or IBD) as a percentage figure derived from our very large study. This is given first for a single symptom, like rectal bleeding alone, then for two different symptoms.
The colour coding reflects the risk – with red being high, yellow intermediate, and white low. We’ve used this structure before across a range of cancers in older people and GPs have found it helpful.
PPVs (95% CIs) for CRC in men and women aged 18 to 49 years for individual risk markers and for pairs of risk markers in combination.
How does the tool calculate the risk of a serious bowel condition?
The research study examined the GP records of over 11,000 patients with cancer or IBD (about six times as many of the latter) plus nearly 27,000 patients without the conditions.
We identified all the relevant symptoms in the year before diagnosis, and compared the two groups. From this – with a help from Bayesian statistics – you can calculate the precise risk when a patient describes the symptoms to their GP.
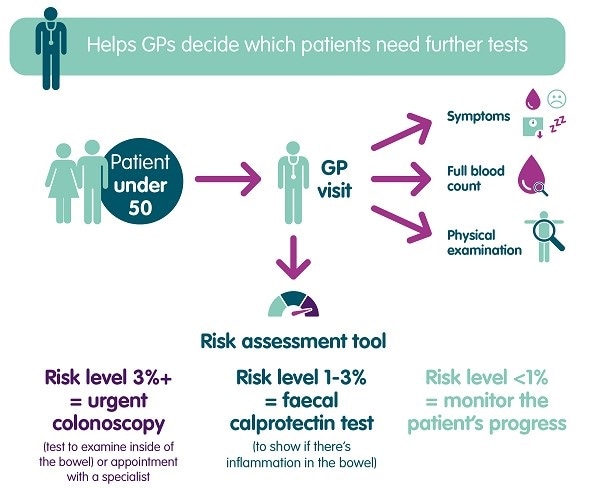
Does the tool suggest next steps?
Sort of – the colour coding reflects the seriousness of the symptoms. But, we aren’t prescriptive. GPs are highly trained individuals – once they have been prompted to the possibility of disease (accompanied by an estimated risk) then it’s up to them and the patient to decide upon the next steps.
What impact is the tool likely to have on the speed of diagnosis?
Similar tools in cancers in older patients appear to be working; times to diagnosis are falling consistently in the UK – some of which can almost certainly be attributed to use of such tools. Even a short period might be enough – especially if it avoids complications/emergency admissions.
What feedback has been received from early adopters of the tool?
This specific tool was launched in April, 2017, so it’s too early to say – previous examples have been widely used however.
Who will the tool be available for?
Primarily GPs, or their professional colleagues in primary care.
Are there any plans to extend this outside the UK?
The family of Risk Assessment Tools have already been used in Denmark, Sweden, and Australia. There’s been considerable interest from the US for this specific tool.
What more needs to be done to raise awareness of serious bowel conditions in people under-50?
This is tricky; it’s a balance between information giving – and being alarmist. The ‘Never Too Young’ campaign of Bowel Cancer UK is doing a great job in raising the profile of young cancer.
Where can readers find more information?
The paper is available from the British Journal of General Practice website.