An interview with David West, CEO and Hunter Jackson, CSO, Proscia, conducted by April Cashin-Garbutt, MA (Cantab)
There have been some barriers to the adoption of digital pathology such as regulatory challenges that are only just now being overcome. Recently, the FDA approved the use of whole slide imaging software for primary diagnostics.
That being said, digital pathology offers a couple of key and core promises that many laboratories are even starting to leverage today. Once you digitize the slide, you can improve operational efficiency, as many studies have shown.
Once the slide is digitized, you're not limited to the physical realm anymore, so it's very easy to move those around: for second opinion consults, for remote tumor boards and so on.
Digital pathology is remarkably useful, and telepathology is where it's starting to be used today, since it's outside of the realm of primary diagnosis.
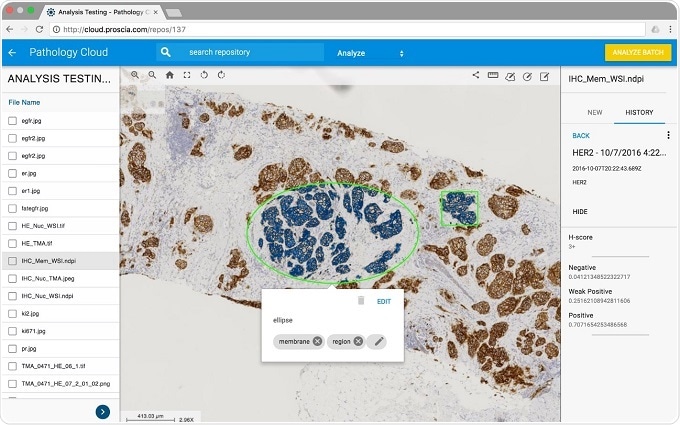
The last of the three key areas, in addition to improving operational efficiency and it being easy to send those slides anywhere, is image analysis, which is what we're particularly excited about.
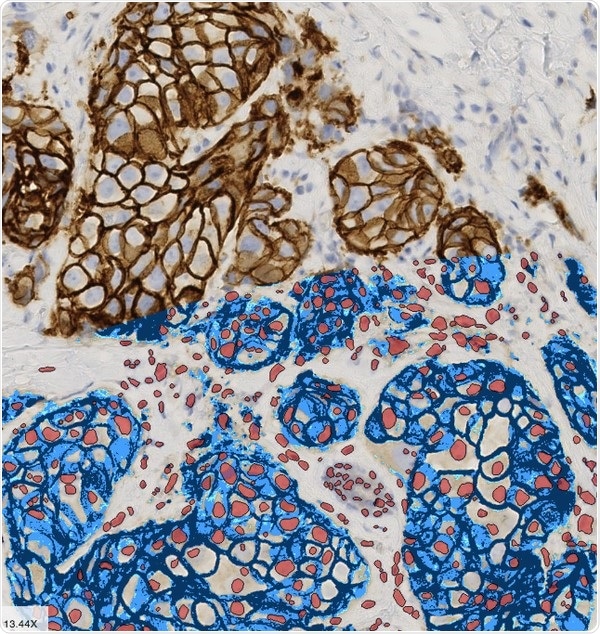
Image analysis has been adopted in the research space for a while for research pathology and drug discovery and so on, but pathology has a lot of challenges in terms of subjectivity and that's where image analysis can play a big role - everything from simple computer vision driven algorithms to more complex and sophisticated algorithms that are in the realm of artificial intelligence.
Hunter: I think David has hit the nail on the head. There is what's going on today and then what's going on tomorrow. I think we're very much focused on both. Some people see a discontinuity with digital pathology and think right now it is not working and that someday it's going to grow up or that right now it's super important, but will then get neglected in the future. I think that we're very much addressing today and tomorrow.
What is Proscia’s vision?
David: Proscia is focused on bringing computational pathology into laboratories. We see a world where pathology is driven by both humans and machines and where software can play a big role. I think that the implications for pathology as a whole is profound.
We're a software company. It's worth noting that a lot of digital pathology is driven by hardware companies and we work with those hardware companies because you have to scan the slide – you have to start somewhere.
We really think that software is the future of pathology, a field that's really been untouched for the last 150 years when it comes to software technology.
What is Proscia doing to bring computational pathology to the lab?
Hunter: We are partnering and collaborating with leading cancer research institutions across the world to train our algorithms to meet FDA standards as a potential tool for primary diagnosis. To do this, we started in one of the most common cancers in the world, breast cancer. By analysing data provided by Radboud University Medical Centre and University Medical Centre Utrecht, we successfully trained our algorithm to predict lymph node metastases in breast cancer patients with 96% specificity and 85% sensitivity. We are currently analysing data to train our algorithms to predict lymph node metastases in lung cancer patients as well and are looking to expand into a wide variety of other cancers.
Recently, we collaborated with five of the top medical centres in the Netherlands as part of the ISBI 2017 CAMELYON Challenge to identify and classify pN-stage in breast cancer patients. pN-stage is a way to measure the extent of regional lymph node metastases in a patient. For the first time our algorithms are producing data at the patient-level, rather than in the lab like previous collaborations. We trained our algorithm to identify and classify pN-stage in breast cancer patients with a kappa score of .776, which exceeds current standards.
Through these collaborations we have a thesis that images could hold the key or the cipher to unlock precision medicine across much broader patient populations than strictly genetic testing does.
Why is accurate prediction of lymph node metastasis so important?
Hunter: When a pathologist is staging a cancer, he or she looks at three main groups: the primary tumor status, the regional lymph nodes and the distant metastasis. We are focusing on the two latter parts of those stages and it's really important to drive precision surgical procedures.
To effectively treat a patient with surgery or neoadjuvant therapy it is really important to understand the extent to which the cancer has spread to lymph nodes and sometimes other organ systems. Pathology and its practitioners are responsible for providing this information, and as it currently stands, most of the genomic and molecular testing do not provide the information needed to make these determinations. Current testing modules are focused on primary tumor status, our algorithms are addressing the metastatic advances of cancer.
Having a predictive biomarker to determine whether the patient's cancer is going to metastasize in the lymph nodes is incredibly important and something that a lot of molecular biomarkers and genomic testing don't determine today. That's why we're focusing on this to start off with and our goal is to build a holistic view of the patient's entire tumor and cancer spectrum using information that we extract from these images.
What have been the main challenges to date in predicting lymph node metastasis and how do you hope to overcome them?
Hunter: A lot of studies in breast cancer and prostate cancer have had great outcomes as a result of genomic testing and molecular biomarkers.
The idea of having a test that can give a much more detailed and personal view of the patient's disease is something that a lot of pathologists and oncologists are very excited about. However, unfortunately, nobody has been successful in developing a molecular or genomic biomarker to predict lymph node metastasis.
We're taking a different view than everybody else. Rather than looking at the genome and the molecular spectrum, we're focusing on the morphology and how the doctor intends to make the diagnosis by looking at the slides.
Our goal is to extract more precisely, more objectively and more consistently and provide similar information, along with extra information, that the human eye can't perceive.

How important do you think AI and machine learning will be in driving precision medicine?
Hunter: The ability to extract pathological features from a patient's tissue sample objectively and consistently is something that has to be driven by AI and machine learning.
Being able to precisely extract those features is what's going to drive precision medicine and I think that this whole space is about people looking at things differently.
There's AI for driving workflow automation and for automating monotonous tasks and as this stands right now, we're very much focused at Proscia on applying AI and machine learning to driving precision medicine for biomarker discovery and eventually for identifying patients for clinical treatment.
David: Taking a step back, the realm that digital pathology deals with is very image-based. If you go back about five years ago or so, there were some techniques in machine learning and image analysis that were good. Then deep learning came along with convolutional neural networks and so forth and people started building very complex algorithms that worked very well on images.
That's been pivotal and when people talk about AI, that's a lot of what is being talked about. It's more complex than that, but at least as it pertains to us, that was one of the really big advancements that suddenly got a lot of the people in our space, including Proscia, to open their eyes and say "Okay, this is possible. This can really happen with the technology that is coming out.”
There's now a lot more computing power and that combines well with this awakening within the pathology space. Suddenly, all these images are being created, when they were previously just physically stuck on pieces of glass.
That confluence has been incredibly exciting and has opened up this entire realm of possibility where we believe, and the data seems to be showing from all these studies that we've done, that the answers are in the images. As Hunter described, the images are like the cipher and able to unlock a lot of challenges that it wasn’t possible to address before. It's exciting.
Do you think digital pathology will become the standard in the future?
David: I do, and I'd go so far as to say that I don't think the term "digital pathology" will exist in a few years. At a certain point, it will be just “pathology”.
We saw that happen with radiology. As excited as we are about digital pathology, I think that’s what we're ultimately going for and we are looking forward to when it's just all digital and that qualifier doesn't even belong.
Where can readers find more information?
https://proscia.com/
About David West, CEO and Hunter Jackson, CSO, Proscia
 David West is the CEO of Proscia Inc., a digital pathology software company. Mr. West founded the company in 2014, and has played a key role in business development, sales, and marketing, as well as the early design and development of Proscia’s software.
David West is the CEO of Proscia Inc., a digital pathology software company. Mr. West founded the company in 2014, and has played a key role in business development, sales, and marketing, as well as the early design and development of Proscia’s software.
Mr. West was responsible for securing $1.2M in outside capital for Proscia to date. He was named by Inc. Magazine as one of the top 50 Global Entrepreneurs Under 25 in 2015. David graduated Johns Hopkins University where he studied Biomedical Engineering with a focus on Computational Biology.
 Hunter Jackson is the Chief Scientific Officer of Proscia Inc., a digital pathology software company. At Proscia, Mr. Jackson leads and manages a team of engineers and research scientists developing image analysis and machine learning algorithms to extract image-based biomarkers for cancer diagnosis.
Hunter Jackson is the Chief Scientific Officer of Proscia Inc., a digital pathology software company. At Proscia, Mr. Jackson leads and manages a team of engineers and research scientists developing image analysis and machine learning algorithms to extract image-based biomarkers for cancer diagnosis.
In addition, he is responsible for establishing and growing partnerships with some of the top medical centers in the world, as well as interfacing with their principal investigators to develop pipelines of cancer-specific diagnostic tools.
Prior to Proscia, Mr. Jackson was a research scientist at the Integrated Mathematical Oncology Lab at Moffitt Cancer Center where he investigated the evolutionary dynamics of cancer by using mathematical modeling of the tumor microenvironment to understand tumor progression and treatment response.
He has also developed computational fluid dynamics software at NASA LaRC and medical software to identify sleep apnea in babies at the College of William & Mary Department of Physics. Mr. Jackson studied mathematics and graduated B.A. (summa cum laude), and M.A. (highest honors) from the University of South Florida. He is on a leave of absence from Ph.D. studies in mathematics at The Johns Hopkins University.