Autism is a clinical diagnosis. There is no one test to diagnose autism. Depending on the type of medical professional diagnosing, typically the DSM-V (standard classification of mental disorders used by mental health professionals in the U.S.) is used to diagnose by primary care physicians, neurologists, and psychiatrists.
Additionally, a set of questions known as the ADI-R (Autism Diagnostic Interview-Revised) and observations in a semi-structured assessment known as the ADOS (Autism Diagnostic Observation Schedule) are typically used by developmental pediatricians.
The most recent numbers show the prevalence of autism at 1 in 68 people. It is higher in males at 1 in 42 while at 1 in 189 in females. Despite this relatively frequent condition, many physicians are uncomfortable diagnosing and managing the symptoms of autism.
Are there other methods that could be used to diagnose autism? Are there genetic tests available?
There are currently laboratory or imaging tests that diagnose ASD. There are an increasing number of genetic mutations that are being linked to autism; copy number variations, for example, which occur more commonly in advanced paternal age.
Patients of genetic conditions such as Rett Syndrome typically exhibit autistic behaviors and meet the criteria for autism. Unfortunately, we don’t fully understand the genetics of autism at this time, however, it is well established that genetic risk factors exist. The risk for a sibling of a child with autism is estimated to be as high as 1 in 5.
At what age are children diagnosed with autism? Could this condition be diagnosed sooner? What holds back accurate diagnoses?
The average age of diagnosis in the US is 4 years, which is unacceptable. Parents often report concerns starting around 12 months old. There continues to be a “watchful waiting” that occurs and then many patients are referred to a specialist for evaluation and diagnosis, however, due to shortages of these specialists especially in rural areas, long appointment wait times and waitlists are very common.
The reason that this delay is so tragic is that there is a very limited window of opportunity in which therapy is most effective. In this early intervention time frame, it has been shown that intensive therapies such as speech and behavioral therapy can later help children with autism transition out of special education classrooms into mainstream education and in some cases with higher functioning patients actually lose the diagnosis and effectively be “cured”.
I have so many personal experiences with this where early diagnosis and intervention have made significant impact for my patients diagnosed with autism and conversely, despite best efforts a later diagnosis and initiation of treatment much less effective.
There are many barriers that hold back an early diagnosis, such as:
- Primary care physicians often do not get adequate training in neurological disorders during residency.
- The diagnosis relies on the recognition of a range of behavioral symptoms that vary greatly from case to case.
- Diagnosis is even more difficult the younger the child is during development, as there is a greater variability the younger the child.
- Autism overlaps with other childhood neuropsychiatric disorders.
- The ADI-R and ADOS are time intensive and require specialized training.
Please give an overview of Cognoa, the machine learning aspects of the platform and the role that it can play in autism diagnosis.
Dr. Dennis Wall, PhD while at Harvard University initially used machine learning techniques to create an algorithm to determine which questions typically used to evaluate children for autism were most predictive.
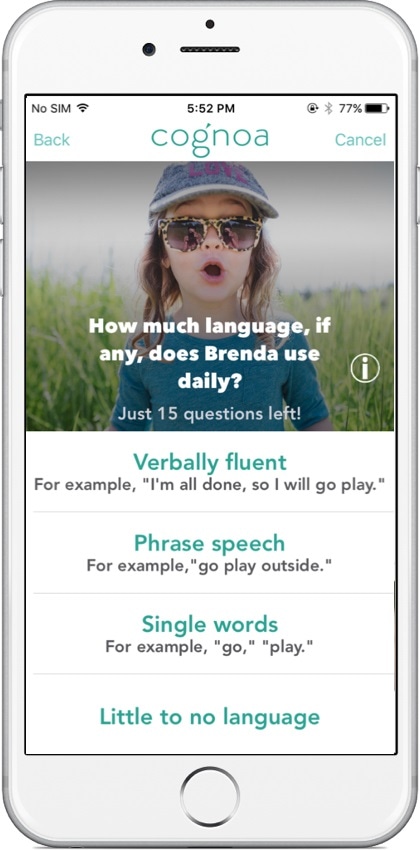
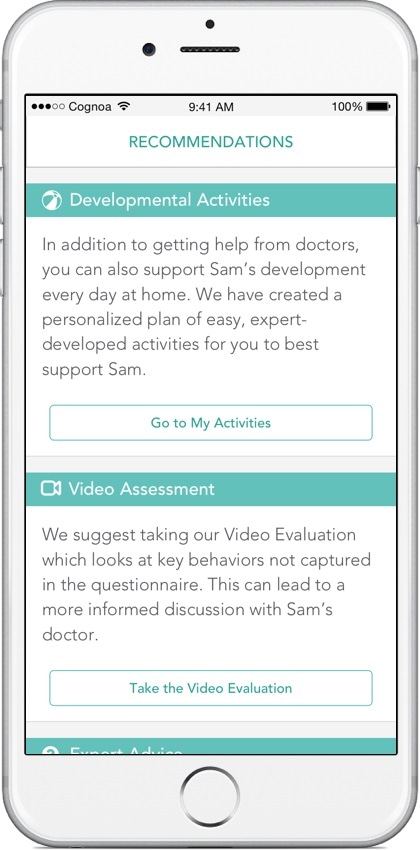
Later, he built upon this work using home videos provided by parents to observe behaviors that were indicative of autism. The team at Cognoa of which he is a co-founder, has expanded on this research to create an advanced algorithm that can empower primary care physicians to make the diagnosis of autism.
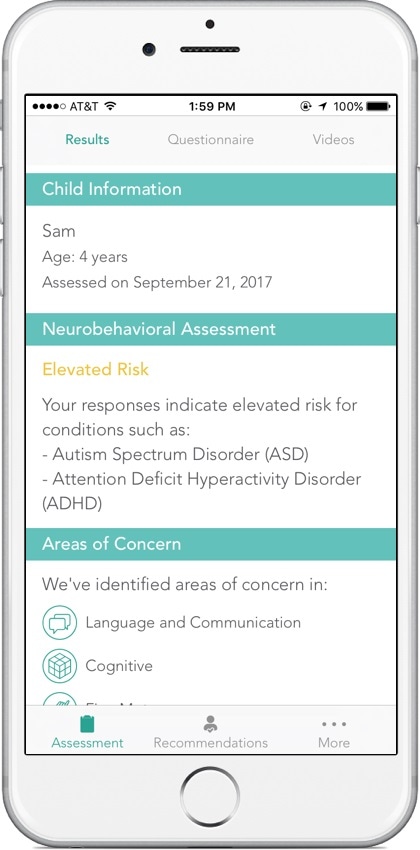
This can significantly reduce the age of diagnosis and in one study, Cognoa correctly identified autism with an average age of 3.08 years old, 13 months sooner than the national average. In analyzing the results from a recent multi-center clinical trial, Cognoa could reduce the number of children that are referred to specialists for autism evaluations by 70%.
Artificial Intelligence has the potential to enhance clinicians’ abilities and I am confident that it will significantly remove barriers and challenges surrounding the diagnosis of autism in the primary care setting.
On what data was the machine learning algorithm modelled? What research supports this program?
The Wall Lab initially used data from Autism Speaks’ Autism Genetic Resource Exchange (AGRE) to create the classifier and then used this same database, in addition to two independent sources (a collection of 1654 autistic individuals from the Simons Foundation and a collection of 322 autistic individuals from the Boston Autism Consortium) to show a high level of statistical accuracy in correctly classifying children with ASD.
Subsequently, Cognoa has continued to work closely with Dr. Wall to advance the algorithm. This improved algorithm was validated through a clinical study conducted at the Thompson Center, Vanderbilt, and the Medical University of South Carolina on over 400 children.
What are the limits to this machine learning approach? How likely is a false positive or a tendency to over diagnose autism?
One of the great things about machine learning is the ability to fine tune the algorithm to take into account real-world prevalence. Meaning that Cognoa is able to provide a different output for children in a primary care practice where the prevalence is 1:68 versus with specialists where the prevalence is closer to 1:30.
We have also built in a safety mechanism that allows the algorithm to say, “I don’t know”. This helps to make sure that when Cognoa flags a child with autism or not, it is as accurate as possible. For those children which Cognoa is not sure if they have autism, they would be referred to a specialist for evaluation.
What does the future hold for the Cognoa platform?
At Cognoa, we are focused on fundamentally changing the standard care for diagnosing and treating behavioral health conditions. Cognoa’s initial product, an assessment for child behavioral development, has been used by 300,000 families and validated in multiple clinical studies and we are actively working to increase both the depth of care we can provide to patients and doctors, as well as the breadth of behavioral health indications we can address.
We engage with clinicians and the FDA to develop diagnostic tools that are integrated with personalized behavioral intervention therapies that parents and doctors can use to ensure that children with delays receive the most effective treatments years sooner than the current system. At the same time, we are expanding our AI and clinical development to increase the breadth of behavioral health conditions we can diagnose and treat.
What advancements in autism diagnosis would you like to see in the future?
I would like to see the average age of diagnosis decrease to around 18-24 months, when early intervention will have the greatest impact. I believe that with Cognoa, we will be able to facilitate accurate diagnosis as early as 12 months.
Where can readers find more information?
To learn more, you can email me directly at [email protected] or visit www.cognoa.com.
About Dr. Taraman 
Sharief Taraman, MD, is the Assistant Division Chief of pediatric neurology and medical informaticist at CHOC Children’s Hospital in Orange County, CA. He is an Assistant Clinical Professor at the University of California, Irvine. He also serves as the Vice President of Medical at Cognoa, a digital health company revolutionizing how children with developmental delays are diagnosed and supported.