A recent study has shown that deadly bacteria such as Pseudomonas aeruginosa behave differently in the humans, compared to a laboratory setting.
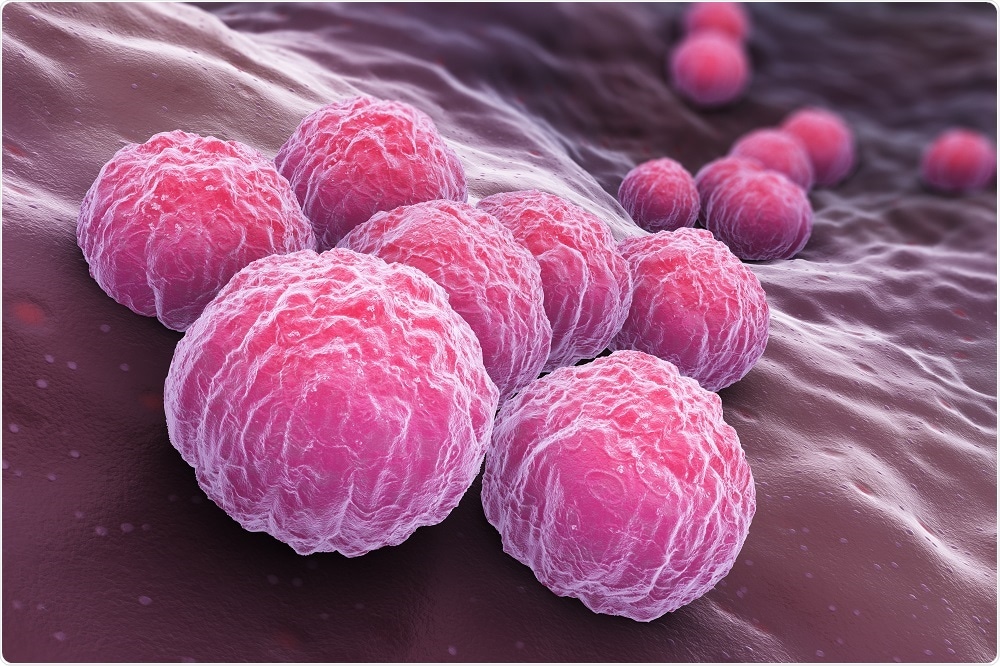
Image Credit: Tatiana Shepeleva/Shutterstock.com
The finding suggests that information obtained from laboratory-based studies may be limited in what it can tell researchers about how the bugs behave once they have invaded humans.
One important difference the study found was that in humans, there was an increased expression of genes responsible for antibiotic resistance.
In this paper, we show that several genes important for antibiotic tolerance are highly induced in humans compared to our laboratory and mouse modeling systems. There appears to be something unique in the human that is promoting resistance."
Professor Marvin Whiteley
Understanding how these genes and their expression levels differ between humans and the laboratory could help researchers establish lab conditions that better mimic human conditions and provide doctors with more accurate information for guiding therapeutic decisions on antibiotic usage.
As reported in Proceedings of the National Academy of Sciences, human samples had high expression levels of several genes notorious for antibiotic resistance, including genes that encode efflux pumps that extrude antibiotics from the cell, as well as an enzyme that degrades certain antibiotics.
There were also less studied antibiotic resistance genes, including three related to zinc transport that our previous work has identified as critical antibiotic resistance determinants that were also highly expressed in the human patients."
Daniel Cornforth, First Author
Although this study focused on Pseudomonas aeruginosa, Whiteley believes the findings could be generalizable to other bacteria and have broader implications. The work could provide a foundation for studying more samples and different types of infection.
Cornforth says the key takeaway from the study is that microbiologists can now perform transcriptomics on bacterial populations in a range of human infections and better understand what the bacteria are actually doing.
"We can also determine where our laboratory models succeed and where they fail in mimicking these infection environments," he adds.