Researchers from the New York Stem Cell Foundation Research Institute (NYSCF) have developed a novel bone engineering technique that could improve treatment for people with bone defects caused by injury or disease.
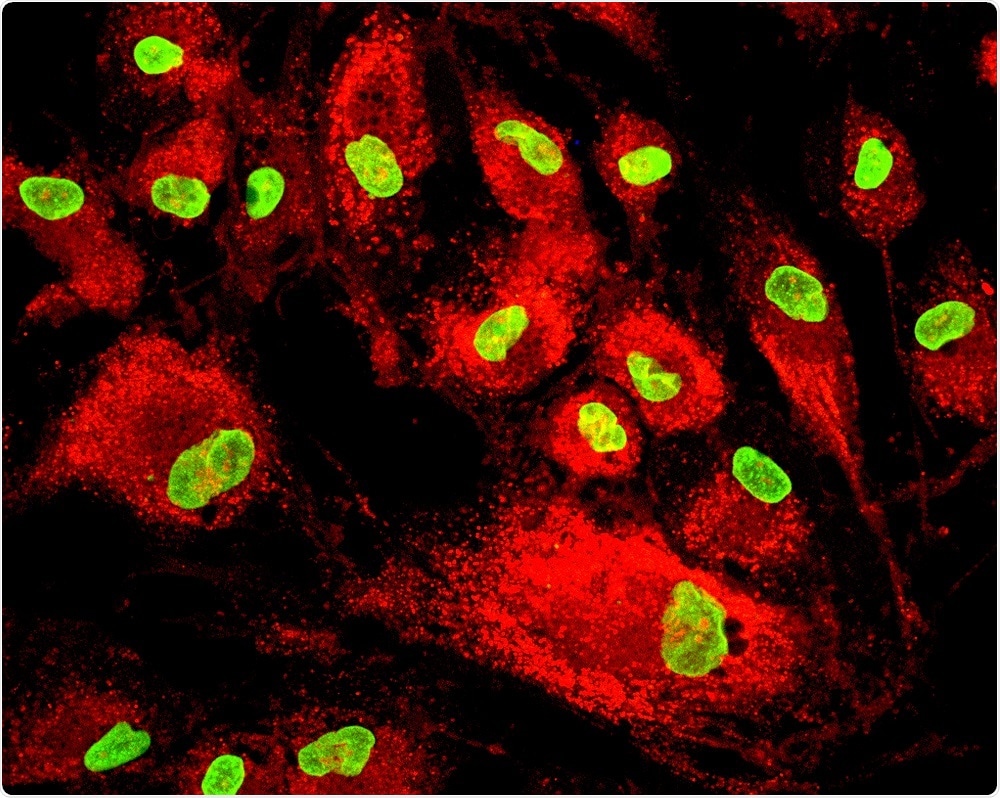 Image Credit: Vshivkova / Shutterstock
Image Credit: Vshivkova / Shutterstock
NYSCF CEO Susan Solomon says the team hopes that the technique, called Segmental Additive Tissue Engineering (SATE), may one day improve the lives of millions of people suffering from bone injury due to trauma, cancer, osteoporosis, osteonecrosis, and other devastating conditions.
Our goal is to help these patients return to normal life, and by leveraging the power of regenerative medicine, SATE brings us one step closer to reaching that goal."
Currently, bone defects are treated with synthetic substitutes or with bone grafts obtained from a bone bank or elsewhere in a patient’s body.
However, these treatments often trigger rejection by the immune system and fail to form the necessary connective tissue or blood vessels. They can also be quickly outgrown in pediatric patients.
Grafts created from a patient’s stem cells do overcome these problems, but are difficult to engineer in the precise size and shape required for large bone defects.
As the size of the defect that needs to be replaced gets larger, it becomes harder to reproducibly create a graft that can move from the lab to the clinic.”
Dr Martina Sladkova, First Author
As reported in Scientific Reports, the SATE technique combines smaller segments of bone engineered from stem cells to produce large, individualized grafts that overcome these limitations in size and shape of grafts that can be grown in the laboratory.
In a rabbit model, the team scanned a defect in the animal’s femur to assess its size and shape and create a model of the graft. The model was then sectioned into smaller segments and individualized scaffolds were formed for each segment.
These scaffolds, which were fitted with human induced pluripotent stem cell-derived mesodermal progenitor cells, were then placed in a bioreactor that was designed to accommodate a range of bone graft sizes.
This bioreactor enabled tissue to develop uniformly throughout the graft. Once cells had grown within the scaffold, bone adhesives or other orthopedic devices were used to combine the individual segments into one mechanically stable graft.
The team are confident this versatile and easy-to-implement technique will one day allow for bone graft engineering that will enhance the treatment and quality of life for individuals suffering from segmental bone defects.