Aug 24 2018
The innate immune response to lung infection takes priority at the expense of wound healing, according to a study published August 23 in the open-access journal PLOS Pathogens by a team of researcher at Brown University led by Amanda Jamieson.
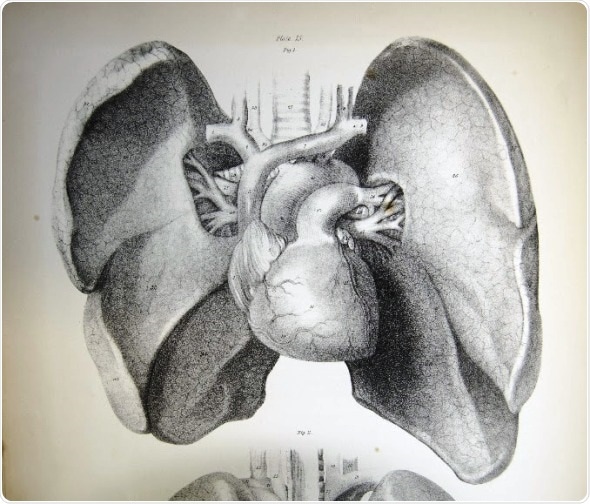
Plate 15 from Jones QUAIN's The viscera of the human body (1840) showing the organs of respiration and circulation - the lungs and heart - anterior view. Credit: University of Liverpool Faculty of Health & Life Sciences, flickr
The innate immune system is responsible for responding to infections, clearing cancerous cells, healing wounds, and removing foreign substances. Although many of these functions happen simultaneously in life, most laboratory studies of the innate (or early) immune response focus on one activity. How the innate immune system responds to concurrent insults in different parts of the body is not well understood. To address this question, Dr. Meredith Crane, Dr. Amanda Jamieson and colleagues set out to determine the impact of a respiratory infection on wound healing.
Mice with skin wounds were infected with the influenza A virus, a common cause of pneumonia. While the innate immune system mounted a response against lung infection, the wound healing response was delayed. The findings suggest that not all immune responses are created equal, and that the cells of the innate immune system are preferentially routed toward fighting a lung infection rather than healing a dermal wound. From a clinical standpoint, altered wound healing could increase susceptibility to further complications in patients. Given the numerous important functions of the innate immune response, the results may have implications for many diseases.
“This study introduces the concept of immune triage, in that when faced with multiple insults the immune system prioritizes responses,” Crane and Jamieson say. “How immune responses to infection, injury, development, or cancer influence each other and the ability to maintain a healthy organism is an important new area of future work.”
“Patients in the hospital with a traumatic injury are at risk of developing pneumonia, which increases morbidity and mortality,” Jamieson continues. “Our work now shows that poor wound healing as a result of a redirected immune response to the lung is another potential co-morbidity, and future work will aim to devise treatment regimens for these high-risk patients.”