Aug 31 2018
The overall mortality in patients suffering non-neonatal tetanus is high. Efforts to reduce mortality in one sub-Saharan African intensive care unit (ICU) by implementing a standard tetanus protocol did little to change mortality rates, although they shifted causes of deaths, researchers have now reported in PLOS Neglected Tropical Diseases.
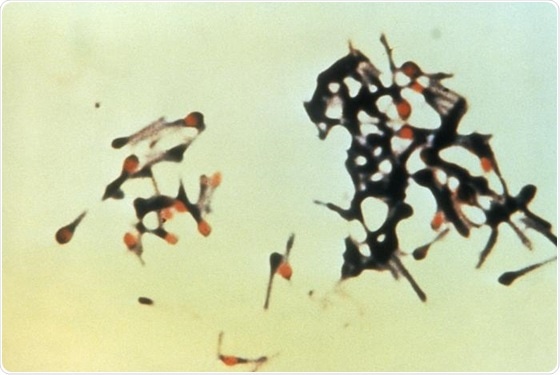
“This micrograph depicts a group of Clostridium tetani bacteria, responsible for causing tetanus in humans. Tetanus is an acute, often fatal, disease caused by an exotoxin produced by C. tetani. It is characterized by generalized rigidity and convulsive spasms of skeletal muscles, usually involving the jaw (lockjaw) and neck, then becoming generalized.”
Credit: CDC Public Health Image Library (Public Domain, 1994)
Tetanus is a vaccine-preventable neglected disease that mostly occurs in regions where vaccination coverage is incomplete. The World Health Organization recommends treating tetanus with patient monitoring, antibody injections, sedation, pain relief, and general supportive care.
In the new work, Jennifer Downs of Weill Cornell Medicine, New York, and colleagues looked at a tetanus patient care protocol implemented in the ICU of Bugando Medical Centre in Tanzania in 2006. The stepwise protocol, which was modified in 2012, emphasized airway control, early administration of medications, and wound care. Patient care and outcomes were analyzed for tetanus patients in three groups—those admitted pre-protocol in 2001 to 2006, those in an Early group, admitted in 2006 to 2011, and a Late group admitted after the protocol was modified, in 2012 to 2016.
The researchers saw a significant increase in utilized care between the Early and Late groups, with more mechanical ventilation, surgical wound care, and tracheostomies used in the Late group. Despite this increase in care, there was no significant change to overall mortality or 7-day mortality between the pre-protocol and post-protocol groups or Early and Late groups, with mortality rates ranging from 40.3% to 60.7% in all groups. There was, however, a decrease in deaths related to airway compromise and increase in deaths due to sepsis in the post-protocol groups.
“Implementation of protocolized care in resource-limited settings is highly complex and requires in-depth monitoring and assessment of patients, staff, and procedures,” the researchers say. “We strongly call from an increase in vaccination coverage for at-risk men in sub-Saharan Africa… with the aim of eliminating this preventable, lethal disease,” they add.