Nov 2 2018
Lymph nodes can contain large numbers of tuberculosis-causing bacteria and serve as long-term reservoirs of bacterial persistence, according to a study published November 1 in the open-access journal PLOS Pathogens by JoAnne Flynn of the University of Pittsburgh School of Medicine, and colleagues. As niches for persistent infection, these organs are likely to play a larger role in tuberculosis than previously appreciated.
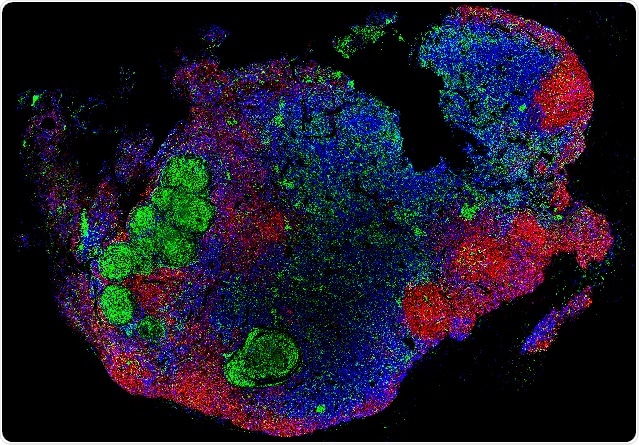
A lymph node with granulomas obtained from a cynomolgus macaque infected with Mycobacterium tuberculosis. CD20 – red; CD3 – blue; CD11c – green. Credit: Ganchua SKC, et al. (2018)
Tuberculosis is one of the significant causes of morbidity and mortality in the world. It is commonly considered a chronic lung disease, and lung infection has been the primary focus of tuberculosis research and treatment. But infection can occur in any organ, and the lymph nodes -- small bean-shaped structures that are part of the body’s immune system -- are among the most frequently infected sites of Mycobacterium tuberculosis (Mtb) – the bacteria that cause tuberculosis. Currently, it is not clear how lymph nodes respond to Mtb infection. To address this question, Flynn and her colleagues examined the effect of Mtb infection on lymph nodes in cynomolgus and rhesus macaques -- two closely related primate species that replicate tuberculosis in humans.
They found that overall lymph nodes are not effective killers of Mtb, especially in rhesus macaques. In contrast, in previous work, the authors found that a large proportion of lung granulomas were quite effective at killing the TB bacilli. Thus, lymph nodes associated with lungs are sites of prolonged persistence of the infection. Mtb infection also resulted in the destruction of the lymph node structure, and this was associated with increased bacterial burden. After a short course of anti-tuberculosis drug therapy, the reduction in bacterial burden was lower in lymph nodes than in the lungs. According to the authors, further research in this area may lead to strategies that improve tuberculosis treatment and patient outcomes. In particular, the findings suggest that lymph node infection should be considered when assessing vaccine and treatment efficacy.