Nov 26 2018
When assessing the effects of socioeconomic status (SES) on health inequalities or outcomes of care, it is worthwhile to use small-area-based open data instead of individual SES information, a new study from the University of Eastern Finland shows. Getting access to individual SES information is often a long and expensive process, requiring many different permits. Published in BMC Public Health, the study found that when predicting the treatment outcomes in patients with type 2 diabetes, the effect of small-area-based SES variables is in line with patient-specific individual SES information.
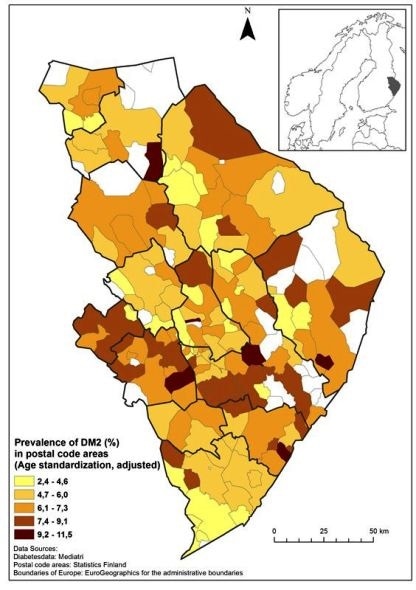
Prevalence of type 2 diabetes by postal code area in eastern Finland in 2012.
This is a significant observation, as small-area-based SES data is available as free, open access datasets,"
Project Researcher Maija Toivakka from the University of Eastern Finland
Small-area-based SES variables can provide cost-efficient first-hand information for health care service planning and proper resourcing. Socioeconomic background information is usually not recorded into clinical electronic patient records, and this is why their use for research purposes is both time-consuming and costly.
Postal code area educational attainment level is associated with outcomes of care
The study explored how small-area-based SES average variables (earned income, educational attainment, unemployment status) and respective patient-specific individual SES information explained treatment outcomes in patients with type 2 diabetes in eastern Finland. The researchers used patients' long-term blood glucose (HbA1c) values as the indicator of treatment outcomes.
The findings show that in postal code areas associated with a lower level of educational attainment, patients had higher long-term blood glucose values. Unemployment status, however, was not associated with long-term blood glucose values neither at the area- nor patient-level. Earned income, in turn, associated differently: high long-term blood glucose values were associated with patients' low earned incomes, but the median income level of a postal code area was not a predictor of patients' long-term blood glucose values.
Various sets of small-area-based data relating to, for example, the built environment are readily available, and these datasets could also be used to predict the prevalence of different diseases, as well as outcomes of care.
The study analyzed data from a regional electronic patient register on 10,204 patients diagnosed with type 2 diabetes, SES variables from a postal code database of Statistics Finland, and patient-specific individual SES variables provided by Statistics Finland.