A new computational model successfully predicts how daily pain sensitivity rhythms affect pain processing, both in healthy adults and in people with neuropathic pain. Jennifer Crodelle of New York University and colleagues present these findings in PLOS Computational Biology.
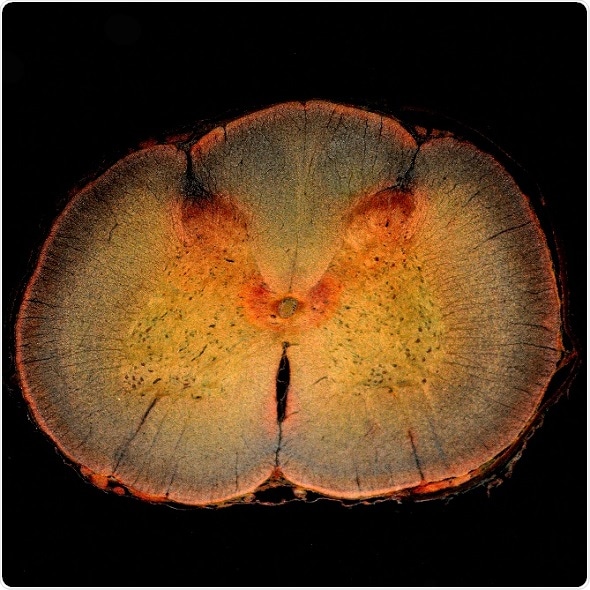
Spinal cord cross section, including the spinal cord dorsal horn, where pain is processed.
Credit: dw_ross/Flickr.
Just as processes like metabolism and alertness exhibit a daily rhythm, pain sensitivity changes over the course of the day. Sensitivity is usually highest in the middle of the night and lowest in late afternoon. However, this rhythm is flipped for people with neuropathic pain, who feel severe pain in response to a typically non-painful stimulus. For these patients, the lowest pain sensitivity occurs at night.
The mechanisms underlying both normal and neuropathic pain rhythms have been unclear. To gain new insights, Crodelle and colleagues built a mathematical model that simulates how pain is transmitted from a nerve to the spinal cord’s dorsal horn, where pain is initially processed.
The researchers found that their model successfully reproduces experimental results on pain sensitivity and predicts how these results are affected by time of day. For instance, it predicts the time-of-day effects on pain inhibition, the phenomenon in which one feels a lessening of pain from applying light pressure, such as by grabbing a stubbed toe.
The model also suggests a potential mechanism for the flipped sensitivity rhythm in people with neuropathic pain: a change from inhibition to excitation in the synaptic connections between nerve cells. This finding points to targets for further experimental study and potential treatment.
Our modeling results provide a first step in understanding how the daily rhythm in pain sensitivity affects normal pain processing across the day and potentially how the daily rhythm can benefit pain management strategies in clinical settings. For example, pain relief medication could be titrated appropriately across the day, thus reducing the total amount of medication needed.”
Jennifer Crodelle, New York University
Potential next steps are to incorporate factors that may influence the daily pain sensitivity rhythm, such as sleep deprivation and jet lag. The model could also aid investigations into how pain sensitivity is reduced by a chronic pain treatment known as spinal cord stimulation.
Source:
Journal reference:
Crodelle, J. et al. (2019) Modeling the daily rhythm of human pain processing in the dorsal horn. PLOS Computational Biology. doi.org/10.1371/journal.pcbi.1007106.