Every living person has trillions of microbes living in their digestive tract, and more than 400 species of bacteria in the gut, more than the number of cells in the body. The normal gut flora is important to maintain eubiosis, the microbial balance in the body.
When there is an imbalance in the gut bacteria, termed as dysbiosis, it can lead to a wide array of digestive disturbances and other health conditions. The gut flora is important in fighting off harmful pathogens, digesting food, and synthesizing vitamins, which all contribute to overall health.
There have been many studies linking dysbiosis to several health conditions. Now, a new study shows that the intake of oral antibiotics can kill the normal flora, altering the human immune response to seasonal influenza vaccination.
A team of researchers at Stanford University, in coordination with the National Institute of Allergy and Infectious Diseases (NIAID), wanted to determine the effect of taking an oral antibiotic to the gut flora and the body’s immune response to flu vaccination. Emerging evidence shows the pivotal role of the microbiome in immunity. But, the studies and evidence in humans are sparse.
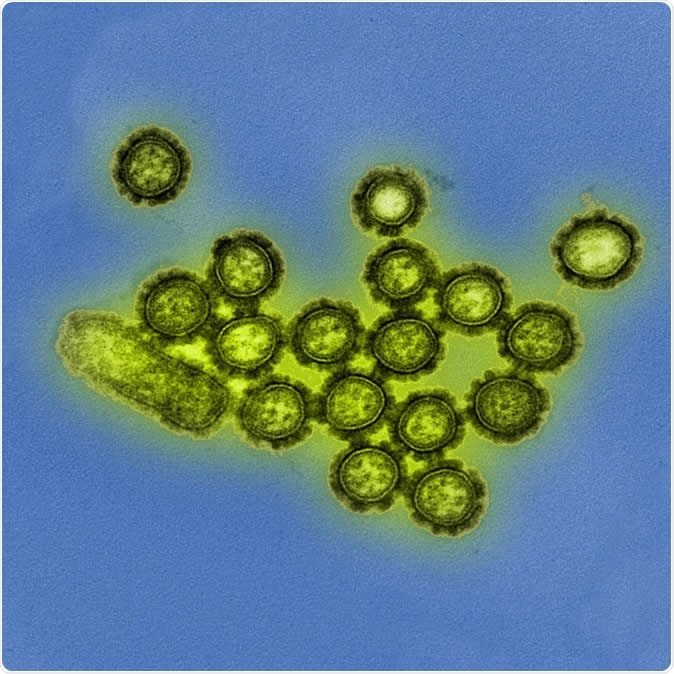
This colorized transmission electron micrograph depicts H1N1 influenza virus particles. Image Credit: NIAID
Administering broad-spectrum antibiotics
To gather the needed data, a team of researchers from Stanford University studied 33 healthy adults. A group of 22 people was studied between the 2-14-2015 flu season, and the second group of 11 participants was observed during the 2015 to 2016 flu season. The first group had high pre-existing immunity to the influenza virus strains in the flu vaccine, while the latter group had low immunity to the corresponding vaccine’s virus strains.
All of the participants received a seasonal influenza vaccine. About half of the participants in each group also received a five-day course of an oral broad-spectrum antibiotic regimen, consisting of metronidazole, vancomycin, and neomycin. After which, they all received the vaccine.
After that, the researchers examined the participants’ stool and blood samples, which were taken and extracted at various times for up to a year after receiving the vaccine. From there, the team tracked and studied the participants’ immune response to the vaccines, including the abundance and diversity of the organisms in their gut flora.
Lower immune response
The results of the study, which was published in the journal Cell, shows that most of the participants who consumed oral antibiotics had decreased gut bacteria. From those from the 2015 to 2016 group, those who had little prior immunity to the seasonal influenza virus vaccine strains, the intake of the oral antibiotics altered and stalled their immune responses to one of three virus strains in the vaccine – an H1N1 A/California-specific virus.
The finding means that if these participants are exposed to the said virus strain, they will be less protected against the infection caused by the specific strain, than those who have not received antibiotics.
The team also discovered that people who consumed antibiotics experienced certain changes in their immune systems, promoting a pro-inflammatory state, just like a condition among older people who have received influenza vaccines. The scientists believe that the effect is linked to the process by which the gut flora regulates or maintains the metabolism of bile acid, with fewer microorganisms.
“Here, we have demonstrated the potential for antibiotic-driven perturbation of the microbiome to influence immune responses to vaccination in healthy adults,” the researchers concluded in the study.
“As antibiotics and vaccines represent two of the most widely used medical interventions, this has important implications for clinical practice and public health. These findings should inform further research seeking to better understand mechanisms that control the interplay between the gut microbiota and our immune system,” they added.
The study findings could shed light on why older adults respond differently to flu vaccines and why they have weaker immune systems or protection against pathogenic organisms.
Journal reference:
Hagan, T., Cortese, M., Rouphael, N., Khurana, S., Golding, H., and Pulendran, B. (2019). Antibiotics-Driven Gut Microbiome Perturbation Alters Immunity to Vaccines in Humans. The Cell. https://www.cell.com/cell/fulltext/S0092-8674(19)30898-0