Researchers in the United States have discovered that many experimental cancer drugs may be missing their molecular targets and are instead succeeding in unintended ways, some of which could have toxic effects.
Using the gene-editing tool CRISPR–Cas9 to investigate how ten cancer drugs interact with their protein target, the researchers found that the proteins are not actually essential to the survival of malignant cells. Seven of drugs the team investigated are currently being tested in clinical trials.
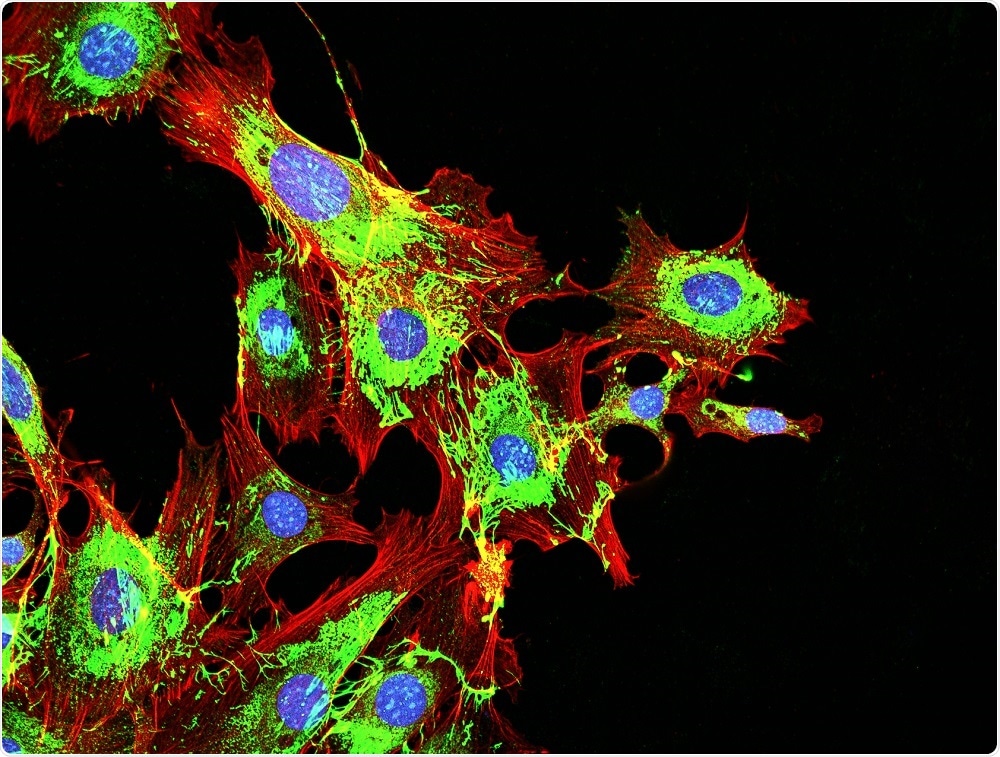 DrimaFilm | Shutterstock
DrimaFilm | Shutterstock
Cancer researcher William Kaelin (Dana–Farber Cancer Institute Massachusetts) who was not involved in the research says the findings could help to explain why many cancer drugs fail in clinical trials:
“The work is very well done and it’s a great public service. I hope people talk about it. I don’t find any of it surprising, unfortunately,” says Kaelin, who has previously written about why promising preclinical findings are often not reproducible or fail to lead to new drugs.
Unintended, unknown targets
The findings do not necessarily mean the drugs fail completely. Some may have proved successful during early studies because they were acting on unintended, unknown targets, explains lead author Jason Sheltzer of Cold Spring Harbor Laboratory in New York.
However, not understanding a drug’s mechanism of action could limit its prospects, he adds. In personalized medicine, a scientist may link a drug to a particular molecular marker that will help to predict how well the therapy would work in a given individual.
Such markers can then be used to select patients for trials who are more likely to respond positively to treatment, which increases the chance of the drug receiving regulatory approval.
However, if a drug’s mode of action is not actually known, then this approach becomes impossible, says Sheltzer. Furthermore, drugs that are targeting unknowns could also be damaging healthy cells, which raises the question of whether they could have toxic effects.
It is hard enough to develop drugs when you know their mechanism of action, but it is really difficult when you don't know the mechanism of action, says Kaelin.
The team made the discovery by accident
Sheltzer and team first discovered the problem by accident while looking for a protein they could use as a positive control in an experiment.
They chose a well-studied protein that was thought to control the division of breast cancer cells. However, when they used CRISPR–Cas9 to cripple the gene that codes for the protein, they found this had no effect on cancer growth.
Curious as to whether this was a one-off or whether the same may be happening with other genes in clinical trials, the team selected ten other drugs for further analysis.
The ten drugs target a total of six proteins and have been used in 29 clinical trials aiming to recruit more than 1,000 people. The six proteins that the drugs target have been implicated in the survival and proliferation of cancer cells in more than 180 publications.
CRISPR versus RNAi
Much of the evidence was generated using a technique called RNA-interference (RNAi), which disrupts a gene’s ability to provide protein-building instructions. Although this method can silence the specific genes it is intended to, it can sometimes also affect the activity of other genes.
Traver Hart of the Anderson Cancer Center in Houston says it now seems that work was “riddled with falsehoods.” Hart now uses CRISPR in his work to look for new drug leads.
However, Kaelin recommends that the results of those studies should be checked using multiple techniques since CRISPR can have off-target effects too: “You have to assume the downstream effects you're measuring are off-target until you prove otherwise.”
For the current study, Sheltzer and colleagues used various different methods to assess the drugs' efficacy. Amongst them was CRISPR–Cas9 — the powerful gene-editing tool that disables genes in a different way to RNAi — by creating mutations in them.
The target proteins had no effect on cancer growth
As reported in the journal Science Translational Medicine, each of the proteins that the drugs targeted had no effect on cancer cells cultured in the laboratory.
Furthermore, When CRISPR was used to wipe out the expression of these proteins, the drugs destroyed cancer cells anyway. This suggests that the drugs work in ways that are not even linked to the proteins they were designed to target.
Next, the team examined one drug in more detail. They found that rather than it exerting its effect on the protein it was intended to, it had targeted a different protein that plays a role in cell division.
The researchers acknowledge that the study has limitations. Co-author Ann Lin (Stanford University) notes that the studies were carried out in cells grown in the lab: “It is possible that these drug targets are essential in human patients,” she says.
'An unexplored world of cancer targets'
Sheltzer hopes the findings could lead to other unintended target proteins being discovered and potentially developed into new cancer therapies.
There is an unexplored world of cancer targets out there. By using CRISPR and other technologies to examine these drugs, we might unlock new targets.”
Jason Sheltzer, Lead Author
Journal reference:
Lin, A., et al. (2019). Off-target toxicity is a common mechanism of action of cancer drugs undergoing clinical trials. Science Translational Medicine. https://stm.sciencemag.org/content/11/509/eaaw8412