The reason why a commonly used range of drugs is not effective in some patients living with Crohn’s disease has so far not been identified. However, a collaboration between the University of Exeter, Royal Devon & Exeter NHS Foundation Trust and the Wellcome Sanger Institute has discovered a genetic marker that could lead to personalized treatments for Crohn’s cases.
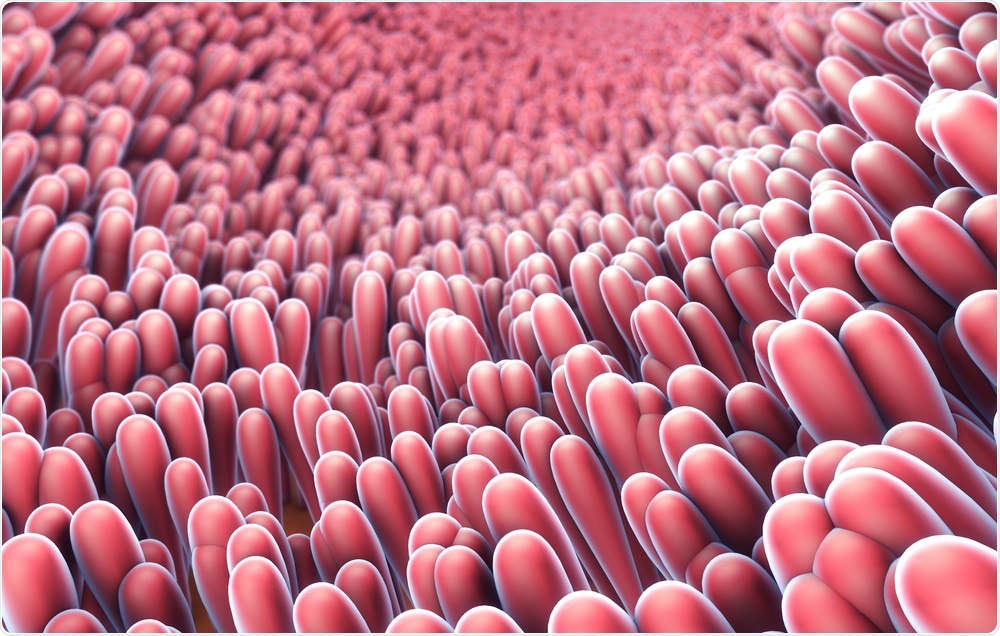 Christoph Burgstedt | Shutterstock
Christoph Burgstedt | Shutterstock
Crohn’s disease is an inflammatory bowel disease-causing inflammation of different areas of the digestive tract in different people. In can cause abdominal pain, severe diarrhea, weight loss, malnutrition, and fatigue, and is a life-long condition.
The study is the largest of its kind and spans the whole of the UK and has found that 40 percent of the European population carries a specific genetic variant that leads to some patients developing antibodies against the anti-tumor necrosis factor (TNF) drugs, infliximab, and adalimumab, causing them to lose efficacy.
Infliximab and adalimumab are widely-used drugs in the treatment of moderate to severe Crohn’s disease and ulcerative colitis when other treatments haven’t proved effective, but many patients find these drugs also lose effectiveness over time. They work by blocking TNF, a cell-signaling protein that is responsible for causing and coordinating the inflammation process in the gut.
The immune system often renders these drugs ineffective
Anti-TNF drugs are made up of large and complex molecules inside living cells. After using the drug for an extended period of time, the body can develop immunogenicity, a process in which the body recognizes a drug as a threat rather than a medicine. This causes the body to produce antibodies that quickly remove the drug from the body and can cause adverse reactions when it is administered.
The Personalized Anti-TNF Therapy in Crohn’s Disease Study (PANTS), published in Gastroenterology, was part-funded by Wellcome, Crohn’s & Colitis UK, Guts UK, Cure Crohn’s Colitis, and supported by the NIHR, and is a part of the program of work focused on discovering the right drug for the right patient first time around.
Tariq Ahmad, Head of the Inflammatory Bowel Disease and Pharmacogenetics Research Group at the University of Exeter, and Consultant Gastroenterologist at the Royal Devon and Exeter Hospital, UK, said the scientists “strongly believe that this type of research is essential to developing cost-effective treatment strategies for patients with inflammatory bowel disease.”
The study researched the clinical data and genetics of 1,240 patients with Crohn’s disease beginning anti-TNF drug treatment at 120 UK hospitals and discovered that the genetic marker HLA-DQA*05 doubles the chances of patients developing antibodies and eventual immunity against anti-TNF drugs.
More therapeutic options for Crohn’s patients are needed
With 160,000 patients living with Crohn’s disease in the UK, the need for fast and effective treatment is clear and the discovery of a genetic marker is particularly significant in the move towards treatment that evades immune responses.
The future of Crohn’s and Colitis treatment is personalized medicine, so the identification of a genetic marker that explains why anti-TNF drugs don’t work for some people with Crohn’s is highly significant. These results are extremely promising and with further research could lead to individualized treatment and better outcomes for the people living with these debilitating conditions.”
Helen Terry, Director of Research, Crohn’s and Colitis UK
A paper published in Gastroenterology & Hepatology in 2015 states that “future therapeutic options will likely include biologic agents that use other mechanisms of action and that are currently on the market for other inflammatory conditions […] as well as other novel approaches working their way through clinical trials.”
It adds that the availability of other groups of effective immune therapies will “allow for more options in the care of patients when biologic agents fail.”
We are delighted to have supported this ground-breaking study. This is an important step towards the goal of personalized medicine for people, around 1 per 200, with Crohn’s disease or ulcerative colitis. We will need a further trial to confirm that genetic testing before treatment will help people with Crohn’s and colitis to get better and more effective personalized treatments.”
Manuela Volta, Research Manager at Guts UK
Source:
Journal reference:
HLA-DQA1*05 Carriage Associated With Development of Anti-Drug Antibodies to Infliximab and Adalimumab in Patients With Crohn's Disease. Gastroenterology.