An interesting letter in the New England Journal of Medicine on November 7, 2019, describes the successful outcome at one year of a rare genital transplant in a young war veteran who lost most of the lower part of the abdominal wall, the scrotum and both testes, and both legs below the knee, to a bomb blast. This is one of only 4 penile transplants reported to have succeeded so far. This procedure is crucial to restoring well-being for male patients, since the loss of these organs has an immense negative impact on psychological, reproductive and sexual function and health.
Left with a 1.5 cm stump of penis and urethra, the patient was treated by a full transplantation of the penis, scrotum, and lower abdominal wall from a donor of similar age. One year afterwards, he was experiencing successful erections and orgasms, indicating that the transplant was working as intended. This complex transplant is the first of its kind in the world, and the doctors have been refining their technique since 2013.
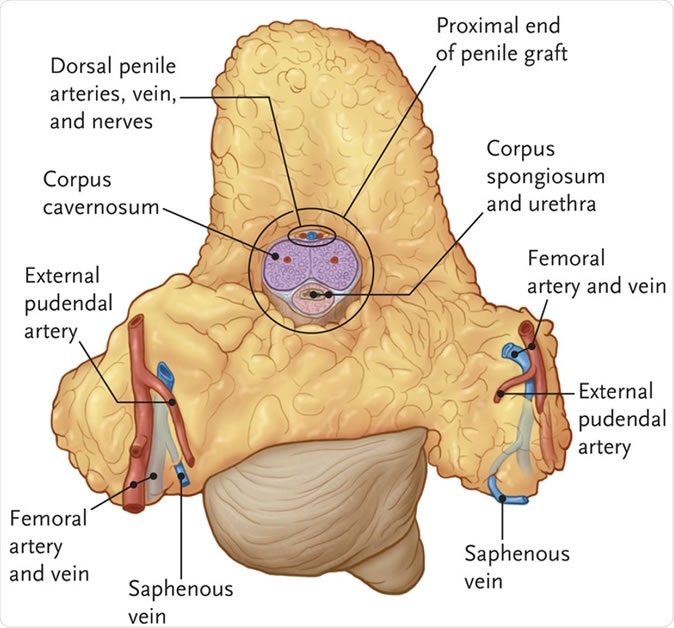
Graft after explantation from the donor. The graft included the right and left external pudendal artery, a segment of the femoral artery, and the saphenous veins on both sides. Dorsal arteries can be seen on the deep, proximal portion of the penile graft. RJ Redett III et al. N Engl J Med 2019;381:1876-1878.
The man had been on a wait-list for the complex procedure, called a “vascularized composite allograft” (VCA), because conventional reconstructive surgery could not have helped him. In addition to tissue and blood type matching, the donor must also have matching skin tone, age and graft organ size. A separate consent is also required from the donor’s family for a VCA which increases the length of the approval process.
The first step of the procedure was to supplement vascular supply to the dorsal penile and cavernosal arteries, which would nourish the transplant. To achieve this, the surgeons connected these vessels to the other intact vessels within the abdomen, with another set of arteries to add supplementary circulation. After repairing the urethra and rejoining it to the penis, the vessels from the transplant were connected to the recipient’s blood vessels, followed by the nerves. The patient did not receive testicles, since that would make it possible for him to father children with completely unrelated DNA, which is unethical by medical standards.
A medical first: Veteran receives genital and partial abdomen transplant
The patient was put on immunosuppressive drugs to prevent any rejection of the transplant, and donor bone marrow transplantation was also performed repeatedly to aid in acceptance of the transplanted tissue. The other injuries were addressed by providing whole leg prostheses.
At the time of writing, the patient could use the penis for intercourse with much greater pleasure, had an almost normal ability to produce and sustain erections, and to reach orgasm. Sensation over the penis is normal, both at the tip and over the shaft. Urination is normal, without urgency or straining. The urine emerges in a full, strong stream and he can urinate in a standing position. Thus the transplant has restored function with respect to urinary, sexual and sensory functions.
The patient is now a full-time student, has a much better self-image, and is satisfied with the outcome of the transplant procedure, including its future implications.
The surgery cost about $300 000 to $ 400 000 to the hospital but the patient received it at no cost. The team plan to do at least 60 penis transplants, and hope for funding from the Department of Defense. They are evaluating several service members for the procedure, which involves a long process of screening, interviews, testing and education. Lead author Richard Redett says, “This is a life-enhancing and not lifesaving transplant, so we are very careful about evaluating the risks and benefits and safety of the procedure.”
W. P. Andrew Lee who heads the department of plastic and reconstructive surgery says, “I think one would agree it is as devastating as anything that our wounded warriors suffer, for a young man to come home in his early 20s with the pelvic area completely destroyed.”
The surgeons published the letter to increase awareness of the possibility of such sensitive transplants with a successful outcome. For instance, there are almost 1400 young war veterans below the age of 35 who suffered genital injuries on duty in Iran and Afghanistan, according to Department of Defense Trauma statistics. About 400 of these had penile injuries, and about 80 injuries were classified as severe. Earlier penis transplants have occurred in South Africa and in the US.
Journal reference:
Richard J. Redett III, Joanna W. Etra, Gerald Brandacher, Arthur L. Burnett, Sami H. Tuffaha, Justin M. Sacks, Jaimie T. Shores, Trinity J. Bivalacqua, Stephen Bonawitz, Carisa M. Cooney, Devin Coon, Aliaksei Pustavoitau, Nicole A. Rizkalla, Annette M. Jackson, Vidhi Javia, Samuel A.J. Fidder, Janice Davis-Sproul, Daniel C. Brennan, Inbal B. Sander, Shmuel Shoham, Nikolai A. Sopko, W.P. Andrew Lee, and Damon S. Cooney. Total penis, scrotum, and lower abdominal wall transplantation. The New England Journal of Medicine, 2019; 381:1876-1878. DOI: 10.1056/NEJMc1907956. https://www.nejm.org/doi/full/10.1056/NEJMc1907956