Can food really be your best medicine? A new review maps how tailored diets could transform public health—if science can keep up with the hype.
 Food as medicine intervention pyramid. Review: Advances in Food-as-Medicine interventions and their impact on future food production, processing, and supply chains
Food as medicine intervention pyramid. Review: Advances in Food-as-Medicine interventions and their impact on future food production, processing, and supply chains
In a recent review published in the journal Advances in Nutrition, researchers explored the concept of ‘Food-as-Medicine’ (FAM), highlighting current trends, challenges, and the impact this concept could have on health outcomes through individualized dietary interventions, processing technologies, and food supply chains.
While FAM appears to reduce healthcare costs by preventing and managing diseases, challenges include individual differences in food response and the difficulty of measuring health benefits. For FAM to succeed, a shift towards health-promoting foods must be encouraged, and technologies and supply chains must adapt accordingly.
Global burden of non-communicable diseases
Public health organizations and researchers increasingly warn of the significant global health and economic burden caused by diet-related conditions such as cancer, diabetes, and cardiovascular disease, which account for 89% of diet-related deaths globally and are implicated in millions of deaths and the loss of trillions of dollars each year. Aging populations, food insecurity, and unhealthy diets worsen these costs.
Extensive research suggests that diet changes can effectively manage or prevent many health conditions. Diets rich in plant proteins are linked to lower mortality and coronary heart disease risk. For example, the BROAD trial demonstrated that whole food plant-based diets significantly improved weight and cholesterol levels. National dietary guidelines, while differing by country, often recommend daily intake of dairy, grains, proteins, vegetables, and fruit, while limiting the consumption of ultra-processed foods. Unlike broad national guidelines, FAM targets high-risk individuals with tailored interventions, such as medically prescribed diets for diabetes management. However, nutrition remains an underused tool in mainstream healthcare.
Now, the FAM approach is gaining attention, integrating traditional concepts with modern technologies like wearables that incorporate artificial intelligence (AI). FAM seeks to promote health, lower healthcare costs, and complement medical treatments, focusing on using whole or minimally processed foods rather than supplements.
The rise of FAM
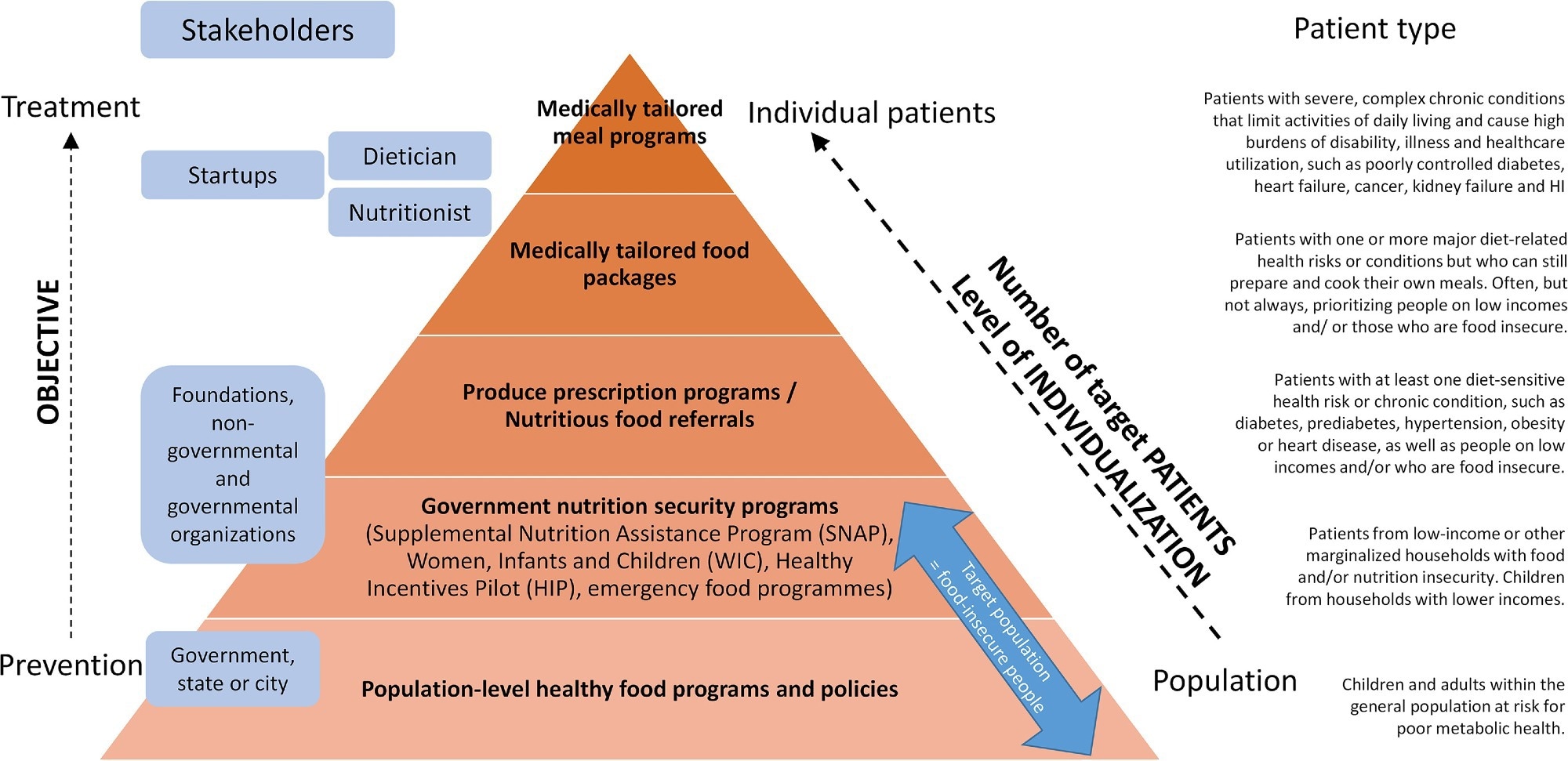
FAM refers to integrating food and diet into health plans to promote wellness, prevent and manage diseases, reduce symptoms, and support conventional treatments. Unlike traditional dietary concepts from Chinese, European, or Ayurvedic medicine, FAM combines nutritional science with modern technologies to reach patients more effectively. The paper outlines a “FAM pyramid” of interventions, a tiered framework starting with medically tailored meals for high-risk patients and scaling up to population-level government nutrition programs. While government programs like SNAP improve food access, their generalized structure limits their ability to address complex medical needs, which require the precision of medically tailored meals (MTMs). MTMs are costly but critical for patients with conditions like renal disease, whereas scalable programs prioritize accessibility over customization.
It targets two main groups: food-secure individuals who consume poor diets and food-insecure communities lacking access to nutritious foods, often leading to higher rates of chronic diseases like diabetes and cardiovascular conditions.
The principle behind FAM emphasizes a balanced diet rich in whole foods, functional foods, and fortified foods rather than relying on supplements. FAM recognizes the physical and psychological benefits of food on mental health and social well-being.
FAM interventions are organized hierarchically, from large-scale programs to personalized treatments. At the top are medically tailored meals designed for patients with serious health conditions. Next are medically tailored food packages and produce prescriptions, which provide subsidized fruits and vegetables to at-risk groups. For example, U.S. trials show produce prescriptions could save $39 billion in healthcare costs and reduce cardiovascular events by 15–30% in high-risk populations.
At a broader level, government nutrition security programs support food access for vulnerable populations. Recent advances have shifted FAM beyond broad guidelines to precision nutrition (data-driven dietary plans) for disease prevention and treatment, leveraging mobile apps, wearable devices, and real-time health monitoring. This differs from “personalized nutrition,” which incorporates individual lifestyles and preferences.
Health insurers also promote healthy eating through apps and reward programs. Overall, FAM is becoming more personalized, scalable, and commercially viable, focusing on whole foods and connecting more individuals directly to expert dietary support through technology.
Impacts on food technology and production
Dietary changes influenced by general guidelines and FAM interventions will shift food production and processing, mainly boosting demand for fruits, vegetables, whole grains, and plant-based proteins.
While broad dietary changes affect large populations, niche FAM interventions like medically tailored meals have smaller impacts. Past examples, like the surging demand for avocados and lemons, show how health perceptions can drastically increase production.
However, scaling up healthy food production faces challenges: global production does not yet meet dietary recommendations, and access remains uneven, especially in low-income and remote areas. The paper highlights the need for postharvest innovations like controlled atmosphere storage and active packaging to reduce waste while preserving nutrients.
Improving the situation would require producing more nutritious foods, reducing food waste, adjusting prices and incentives, and decreasing reliance on unhealthy foods. Expanding supply chains – especially refrigerated "cold chains" – will be necessary but could increase environmental impacts. Innovations to preserve food quality and reduce waste are crucial, especially since FAM may require more specialized food products.
Making FAM effective
The effectiveness of FAM treatments depends on factors like a patient's health, food availability, costs, environmental impacts, and especially adherence to the diet. Key challenges include bioavailability (how well nutrients are absorbed), financial support for patients, cultural and lifestyle barriers, and maintaining motivation through visible health improvements.
Food-drug interactions and food processing also affect outcomes, as structure and chewing influence nutrient uptake. Food processing methods, such as fermenting or milling, can enhance or degrade nutrients, underscoring the need for tailored preparation in FAM interventions. Long-term adherence is often needed for lasting effects. The paper stresses that individualized FAM approaches lack robust clinical validation and require long-term cost-benefit analyses. Additionally, there is a shift toward personalized FAM approaches targeting patient groups rather than individuals, though full individualization remains challenging and costly due to genetic, environmental, and dietary complexities.
Like personalized medicine, tailoring an entire diet for one person requires vast data and months of tracking, making it difficult for widespread application. Despite these hurdles, segmentation and personalization are seen as promising directions for improving FAM interventions.
Conclusions
FAM has strong potential to prevent and manage diseases, lower healthcare costs, and shift food production towards healthier options. Successful FAM implementation needs better physician support, technological innovation, and responsible actions by governments, industry, and academia to promote healthy, sustainable diets and integrate food into mainstream healthcare. The authors emphasize the FAM pyramid as a roadmap for scaling interventions and call for clinical trials to validate individualized approaches.
Journal reference:
- Advances in Food-as-Medicine interventions and their impact on future food production, processing, and supply chains. Defraeye, T., Bahrami, F., Kowatsch, T., Annaheim, S., Bragt, M.C.E., Rossi, R.M., Greger, M. Advances in Nutrition (2025). DOI: 10.1016/j.advnut.2025.100421, https://www.sciencedirect.com/science/article/pii/S2161831325000572?via%3Dihub