The microbes in the gut comprise several trillion species that are involved in various metabolic reactions, including the absorption of nutrients, regulation of energy levels, and the immune response. One of the metabolites produced by gut bacteria from the digestion of animal nutrients, especially choline and carnitine, in the gut is trimethylamine N-oxide (TMAO).
L-carnitine is richly found in red meat and other animal meats and is useful as a fatty acid transporter into the mitochondria for beta-oxidation. However, it is also a suitable food for many bacteria in the gut.
TMAO has been related to an increased risk of coronary heart disease, which can result in heart attacks. On the other hand, a vegan or vegetarian diet is linked to a low TMAO production in the body.
Earlier research shows that high TMAO levels increase the rate of atherosclerosis. And more, as the intake of red meat increases, the amount of TMAO-producing bacteria in the gut goes up, changing the gut microbiome pattern. The reverse is true when switching to a plant-based diet.
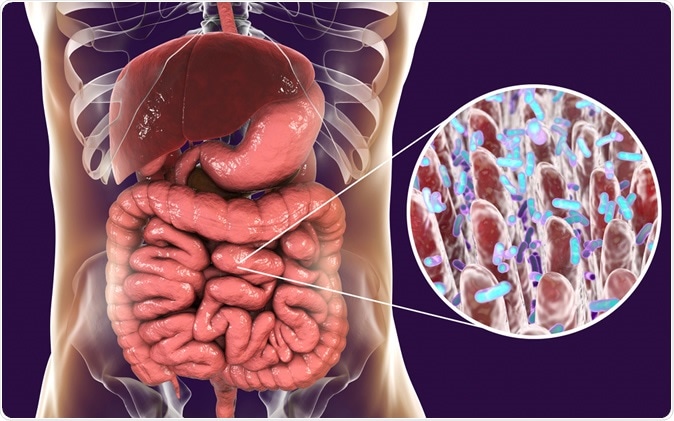
Intestinal microbiome, anatomy of human digestive system, 3D illustration Credit: Kateryna Kon / Shutterstock
The study
The researchers looked at dietary data from 760 women enrolled in the Nurses’ Health Study, which is a prospective cohort study involving over 120,000 registered female nurses aged 30 to 55 years. They also reported their smoking and exercise patterns, and provided two blood samples each, at an interval of 10 years.
The researchers looked at the plasma concentrations of TMAO and how it changed from sample 1 to sample 2. There were 380 cases each of individuals with and without CHD, but both groups had good matching with respect to demographic characteristics. That is, they were otherwise similar.
The investigators calculated the change in the TMAO level over these ten years, making allowance for the fact that TMAO levels also depend on the diet and the nutrient intake. They aimed to find out how the diet affects the linkage between TMAO and CHD.
The findings
The researchers found that at the time of the first sample collection, there was no difference between the groups in terms of TMAO levels.
However, the TMAO concentrations showed an upward trend in the groups with CHD after 10 years. Each level of increase in TMAO was linked to an increase in CHD risk by 23%.
The women who developed CHD had higher TMAO concentrations, but also a higher body mass index (BMI). These women also had a family history of heart attack and followed a relatively unhealthy diet, including a higher vegetable intake and more animal-based foods.
They then controlled for demographic differences, differences in diet, and lifestyle, but found the linkage remained constant.
When they compared women with the highest and lowest TMAO levels, the risk of CHD was 67% higher in the former relative to the latter.
Implications
Investigator Lu Qi says, “No previous prospective cohort study has addressed whether long-term changes in TMAO are associated with CHD and whether dietary intakes can modify these associations. Our findings show that decreasing TMAO levels may contribute to reducing the risk of CHD, and suggest that gut-microbiomes may be new areas to explore in heart disease prevention.”
Other experts consider that the study confirms the role of TMAO as a biomarker that can predict the risk of heart disease. Moreover, it supports the need to intervene to reduce TMAO to reduce the heart disease odds, as earlier studies have suggested. Says Stanford University School of Medicine professor Paul A. Heidenreich, “The results should encourage us to continue to advocate for more widespread adoption of healthy eating patterns.” This includes a mostly plant-based diet with plenty of fruits and vegetables, whole grains, fish and poultry, and low amounts of red meat and processed meats.
The study has some limitations, including the self-reported data, which may have introduced a bias. Secondly, it is based on women alone, and women who are health professionals, which limits the generalizability of the findings.
More research is needed to validate the association between TMAO and CHD, and to cover a sample that is more representative of the US population at large.
Journal reference:
Yoriko Heianza, Wenjie Ma, Joseph A. DiDonato, Qi Sun, Eric B. Rimm, Frank B. Hu, Kathryn M. Rexrode, JoAnn E. Manson, Lu Qi, Long-Term Changes in Gut Microbial Metabolite Trimethylamine N-Oxide and Coronary Heart Disease Risk, Journal of the American College of Cardiology, Volume 75, Issue 7, https://doi.org/10.1016/j.jacc.2019.11.060.