Desperate times need desperate measures. Accordingly, scientists, today published a new study in the journal Cell Host and Microbe in March 2020, showing that drugs that prevent the acquisition of DNA-borne antibiotic resistance traits from their surroundings by bacteria can stop mice from becoming resistant to the action of the antibiotics.
There are millions of resistant bacteria causing severe and, in many cases, untreatable infection in the world today, reminding many scientists of the days before the modern antibiotic era. It is calculated that antibiotic resistance causes $20 billion in additional healthcare costs and a $35 billion loss due to reduced productivity. About 700,000 patients die each year due to antibiotic resistance, which has been found to occur in most bacteria species, often to multiple drugs and sometimes to all known drugs. By 2050 Antibiotic resistance-related fatalities could rise to 10 million people.
Becoming competent
The ability of a bacterium to pick up genetic characteristics that lead to its resisting killing or inactivation by antibiotics is called competence. The current study showed that drugs that inhibit this competence in the common bacterium Streptococcus pneumoniae could keep the animal hosts, namely, mice, alive and well. The key point is that this competence is arrested, but the bacterial cells continue to grow. This makes it difficult for bacteria to acquire resistance traits.
Streptococcus pneumoniae
S. pneumoniae is a typically harmless commensal organism in the human nose and throat. Occasionally it becomes virulent, such as when it travels to other parts of the body to induce serious disease manifestations. Antibiotics are then essential to treat the infection and eliminate it or bring it under control until the immune system inactivates the bacteria.
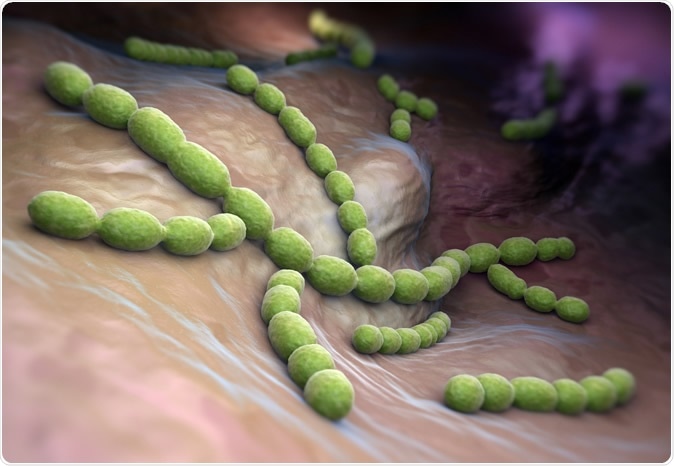
Streptococcus pneumoniae. Gram-positive coccus shaped pathogenic bacteria. Image Credit: Tatiana Shepeleva / Shutterstock
However, when antibiotics are started, these bacteria may acquire resistant characteristics. This is when the hostile situation, involving the presence of an antibiotic compound that is toxic to the bacterium, triggers the cascade of processes that lead to bacterial competence. In simple terms, this means just that the bacteria learn to cope with this stressor by synthesizing some more cellular machines that can sense and acquire genes that will help the cell to become invulnerable to that antibiotic, and incorporate those genes into its own genome.
In an earlier study, Domenech et al. showed that when drug-resistant bacteria are treated with some common antibiotics, they formed long chains instead of the typical mother cell-daughter cell pairs. The chain-forming bacteria reached competence at different times, effectively prolonging the duration of competence. Drugs that stimulate chain formation also often stimulate the formation of biofilms, in which the bacteria produce sticky films to protect them against immune cells.
The study
The challenge that faced the researchers in the current study was how to stop this process, whereby the bacteria became competent. The first step was to find out which bacteria had developed competence and which were actively growing at the same time. This was crucial to executing the novel strategy they had thought up, which was based on an observation they had made.
Says investigator Arnau Domenech, "'When cells are under growth stress, for instance, in the presence of antibiotics, they try to find a solution and become resistant to these drugs." The key was, therefore, finding antibiotics that would not put the bacteria under growth stress conditions.
To do this, says Domenech, "We collaborated with scientists from Heidelberg, who developed a high-throughput assay to simultaneously test cells for competence and growth." They exposed the growing bacteria to 1366 approved drugs to screen them for the acquisition of competence during this growth phase.
The findings
The results were satisfying. They found that with 46 of the tested drugs, the bacteria failed to become competent but continued to grow. These included drugs in two categories: those which prevented the cell from maintaining the proper balance of ions inside and outside the cell, and those which were used to treat psychotic conditions.
Domenech explains, "Importantly, we did not observe resistance to the drugs found here as they do not cause growth stress."
The next step was to weed out the less promising candidates. The researchers found that all the best-performing candidate drugs worked the same way since they all belonged to one of two drug groups only. The mechanism of action was the disruption of the proton-motive force. This refers to the electrochemical gradient, the physicochemical force that transports protons across the cell membrane of the bacterium and supplies the power for the various cellular processes.
How it works
The failure of this mechanism in the presence of these drugs causes a definite change to occur: "The cells fail to secrete a peptide called CSP," says Domenech. As a result, the concentration of competence stimulating peptide (CSP) outside the cell falls. A normal CSP concentration is necessary to induce competence through a phenomenon called 'quorum sensing', that is, the bacteria sense, from the total CSP level, whether or not enough of them are secreting CSP before activating their competence genes. If so, all the cells become competent almost simultaneously.
As the workers watched, they saw that these drugs successfully blocked the acquisition of competence and thus the transfer of antibiotic resistance genes to antibiotic-sensitive strains of S. pneumoniae. They then repeated the experiment with human lung epithelial cells. Says Domenech, "We obtained the same results in cultures of human lung epithelial cells.'
The drugs screened in the current study were used at low concentrations, even lower than that necessary to inhibit growth. This explains their unique growth-sparing but competence-inhibiting activity. However, their safety in humans is still not established. Because the proton-motive force is in high demand even for non-disease pathways, safety studies have to be done to examine just how much this finding helps to tackle the vast and growing problem of antibiotic resistance.
Implications
If successful, the scientists have a fruitful research avenue ahead, identifying competence blockers which prevent the development of competence and thus make it possible to treat a plethora of infections which are now resistant. If there were a combination of this type of drug with the usual antibiotics, it would be a very potent tool to extend the reach of antibiotics for many more years and make it possible to fight many more infections successfully.
Journal reference:
Arnau Domenech, Ana Rita Brochado, Vicky Sender, Karina Hentrich, Birgitta Henriques-Normark, Athanasios Typas, Jan-Willem Veening, Proton Motive Force Disruptors Block Bacterial Competence and Horizontal Gene Transfer, Cell Host & Microbe, 2020, https://doi.org/10.1016/j.chom.2020.02.002.